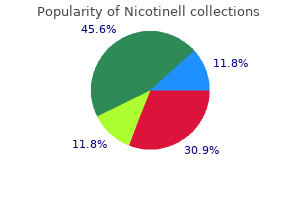
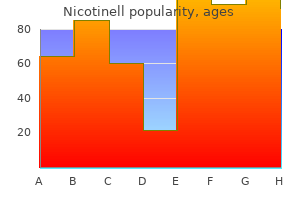
Nicotinell dosages: 52.5 mg, 35 mg, 17.5 mg
Nicotinell packs: 1 packs, 2 packs, 3 packs, 4 packs, 5 packs, 6 packs, 7 packs, 8 packs, 9 packs, 10 packs

Discount 52.5 mg nicotinell with amex
It is commonly unwell defined and, within the chronically sprained ankle, could additionally be manifest as a capsular growth. The anterior margin of the talus is wider than the posterior margin, which makes the ankle extra susceptible to inversion injuries while in plantarflexion. Duration of symptoms, the kind of incidents that cause sprains, the necessity for useful bracing, and former remedies are important for determining remedy recommendations. If ache is current between episodes of instability, different lesions in regards to the ankle must also be thought of. Anterior translation 5 mm higher than the contralateral ankle, or an absolute value of higher than 9 mm is suggestive of instability. Stress radiographs could also be helpful, however physical examination remains the gold standard for analysis of instability. Proprioceptive coaching and peroneal tendon strengthening are the most important options. This is most helpful within the acute setting to decide which buildings are injured. The ankle is held in plantarflexion, and the talus is translated forward relative to the tibia. A talar tilt angle higher than 10 levels, or 5 levels higher than the contralateral ankle, is taken into account pathologic laxity. With the nonoperated leg protected, a platform may be used to facilitate positioning of the operated leg. Alternatively: positioning within the lateral decubitus position, utilizing a stack of folded sheets to function a relaxation for the operated leg. The length of therapy varies based on power deficiencies and the intensity of the program. Orthotic devices and shoe put on modification can be used when foot or ankle malalignment contributes to the instability. A relative contraindication for this anatomic restore is generalized ligamentous laxity as might be encountered in Ehlers-Danlos syndrome. If an osteochondral lesion is current, the ligamentous reconstruction should be carried out in conjunction with arthroscopic or open remedy of the osteochondral defect. This strategy facilitates access to the peroneal tendons should there be related peroneal tendon pathology. The affected person is positioned as described, a thigh tourniquet is positioned, and a normal orthopaedic prep and drape is carried out. With the bump positioned proximal to the ankle, a dissection is carried out to isolate the inferior extensor retinaculum. The joint capsule is then incised according to the pores and skin incision and just distal to the forefront of the fibula. This inspection, together with the preoperative analysis, is used to determine whether or not a restore of this ligament is needed. A subperiosteal dissection is carried out at the anterior and lateral facet of the fibula, raising a flap three to 6 mm extensive. Using curettes and rongeurs, a trough is made in the anterior and lateral facet of the fibula at its leading edge, about 3 mm deep and three mm broad. If further shortening is needed, the capsule could additionally be trimmed from the distal minimize edge. A second reinforcing layer of repair is created by suturing the inferior extensor retinaculum to the periosteal flap with absorbable 2-0 figure 8 sutures. The skin is closed in layers with 3-0 absorbable suture within the subcutaneous suture and staples or subcuticular suture used in the skin. Modified Brostrom Anatomic Lateral Ankle Ligament Repair with Suture Anchor(s) (Courtesy of Mark E. Lift the limb by the anchors; if the anchors are going to fail, we would like them to achieve this now so the problem can be rectified. Mobilize the inferior extensor retinaculum to be used to augment the restore (Gould modification of the Brostrom procedure). Stability of suture anchors tested by lifting limb from the operating room desk by the anchor sutures.
Nicotinell 52.5 mg free shipping
Other circumstances corresponding to ossification of the posterior longitudinal ligament, trauma, infection, and neoplasm can end result in stenosis that could be handled with laminoplasty. The key to treating this condition is to achieve multilevel decompression that alleviates circumferential compression and permits the spinal twine to drift away from ventral compressive lesions. The degenerated discs are extra fibrotic on account of proteoglycan loss throughout the nucleus pulposus. This is associated with lost water content from the nucleus pulposus and lack of regular shock-absorbing capability. With disc degeneration, the disc height decreases and the annulus fibrosus bulges radially, leading to ventral spinal canal narrowing. Collapse and loss of lordotic curvature can result in a cascade of compensatory adjustments, together with osteophyte formation around the uncovertebral joints, the side joints, and the insertion of the annulus fibrosus. Protruded disc materials, osteophytes, and thickened gentle tissues throughout the canal or foramen end in extrinsic stress on the nerve roots or spinal cord. Spondylotic adjustments and osteophyte compression can also impair the circulation within the cord, leading to twine ischemia and resultant myelopathy. This is due partly to the truth that most instances now are handled surgically and early studies of the disease happened several a long time in the past. At that point fashionable diagnostics had been unavailable; subsequently, confounding variables because of different neurologic circumstances cloud the picture. What is understood about the natural historical past is that the disease course of progresses in a variable and unpredictable method. Sensory symptoms may be transient, however motor symptoms tend to persist and progress. The occiput�C1 articulation is answerable for 50% of neck flexion and extension and the C1�C2 atlantoaxial articulation is liable for 50% of whole rotation. Lateral bending below the C2�C3 stage is coupled with rotation because of the 45-degree inclination of the cervical facet joints. The subaxial vertebral segments of C3�C7 are similar to each other and distinct from C1 (atlas) and C2 (axis). The subaxial vertebrae articulate by way of zygapophyseal or aspect joints posteriorly and laterally by way of the uncovertebral joints, or joints of Luschka. Pain is incessantly not a big criticism in myelopathic patients unless related to root compression or aspect arthrosis. On the motor examination, relying on the level of wire compression in addition to nerve root and peripheral nerve dysfunction, mixed upper and lower motor neuron findings may be present within the extremities. The Lhermitte signal is said to be optimistic when extremes of neck flexion or extension end in paresthesias and weak point. Pathologic reflexes such because the scapulohumeral reflex (indicates compression above the C3 level), inverted radial reflex (indicates compression at the C5 to C6 levels), the Hoffman sign, clonus, the Babinski signal, and finger escape may be current. Flexion and extension views can provide details about attainable spinal instability. They could report burning ache in the upper extremities, difficulty in handwriting and fine motor management, diffuse numbness, and weakness of grasp. Advanced instances can current with flaccid weakness and bowel and bladder dysfunction. The bodily examination should start with an assessment of gait, which may be wide-based, hesitant, stiff, or spastic. Patients could also be unable to carry out heel-toe walk or might have poor balance during toe raises. Preoperative lateral cervical spine radiograph demonstrating spondylotic modifications: diffuse disc peak loss and osteophyte formation. Ossification of the posterior longitudinal ligament Peripheral neuropathy or nerve injury Drug intoxication Vascular illness Autoimmune disorders anatomy of the dorsal cortices could be helpful. If concomitant fusion is deliberate, the midline splitting laminoplasty ("French door") method may be considered, but a unilateral open door technique can be used with fusion and lateral mass instrumentation.

Generic nicotinell 17.5mg mastercard
This typically results in shortening of the Achilles tendon and equinus contracture. In the sagittal (lateral) airplane this results in loss of the longitudinal arch at the midfoot, with a midfoot sag. A plantigrade foot balances relatively evenly on the weightbearing surfaces of the primary and fifth metatarsals and the heel. When the midfoot collapses, this stability is disrupted and weight bearing ultimately may be on the midfoot as properly. Also, a affected person with neuropathy might develop midfoot destabilization but without recollection of trauma or with a historical past of what appeared to be solely a minor trauma. Patients expertise ache with weight bearing, especially with push-off during the gait cycle. With advanced disease, lack of the longitudinal arch and forefoot abduction are present. Midfoot tenderness and ache with stress Tenderness is usually targeted on the midfoot. The "piano key test" isolates the focus of the pathology to the specific tarsometatarsal joint. Preoperative Planning Preoperative weight-bearing radiographs of the foot are essential to determine the preoperative plan. The diploma of destruction or distortion of the midfoot anatomy (particularly with erosive adjustments of an inflammatory arthropathy) is essential and elements in how to finest reconstruct the midfoot. Equinus contracture the preoperative assessment should embody the situation of the Achilles tendon. Often Achilles lengthening, both with a triple cut or gastrocnemius-soleus recession, is important to realign the foot and should serve to unload stresses on the midfoot. Equipment Various screw and plating systems, some even dedicated to the midfoot, are available. Procedures might embody arthrodesis in situ or arthrodesis together with realignment midfoot osteotomy. Occasionally, adjunctive hindfoot procedures and Achilles tendon lengthening may be warranted. Rongeur in junction between base of second metatarsal and first cuneiform (it is important to ensure the second metatarsal totally reduces). Note that the windlass mechanism remains to be being maintained with dorsiflexion of the toes. Large bone reduction clamp to make positive that the second metatarsal base is decreased, very related to open discount and inside fixation of an acute Lisfranc fracture-dislocation. Provisional fixation for second metatarsal is the guide pin for the drill for the screw to be positioned from the first cuneiform to the second metatarsal base, a conventional "Lisfranc screw. Note that the guide pin position was checked on fluoroscopy and measured to decide optimal screw length, and then the information pin was pushed totally via the second metatarsal to exit the lateral wound. This means, when the guide pin is drilled and probably sheared by the drill, each ends of the guide pin may still be retrieved. Before inserting definitive fixation, the surgeon ought to examine the stability of the forefoot (metatarsal heads). Metatarsal heads must be well balanced, with the sesamoids slightly more plantar than the second and third metatarsal heads. Using a bone reduction clamp as for open reduction and internal fixation of an acute Lisfranc fracture-dislocation may be useful. I measure the specified screw length after which move the wires all through the foot. While performing provisional fixation, remember that the metatarsal heads have to be balanced. I routinely use solid screws however could provoke the drill hole with a cannulated system.
Cheap nicotinell uk
There is a notch on the lateral and medial wall of the cutting block to show the level of the joint. First insert the stabilizing pin on the proximal-medial side of the cutting block to ensure that the medial-lateral placement of the block will take equal bone from the medial and lateral malleolus (about one third of the width). With enough placement of the slicing block, insert one or two more stabilizing pins. Perform the tibial, tibial keel, malleolar, and talar bone cuts utilizing the respective slots within the slicing block. Remove the chopping block and if needed full the nook cuts with a reciprocal saw. Remove the distal tibial bone, taking care to not rotate the fragments, as it can put extra pressure on the malleoli. To enable placement of the burr information, take away the distraction gadget to enable full plantarflexion of the ankle. Then place the burr information centered on the minimize surface of the talus, with the alignment jig parallel to the second metatarsal. Before securing the chopping block to the tibia, saw blades are used to confirm that equal amounts of tibia and talus shall be removed. After removal of the bone from the tibia and malleoli, the burr guide for the talar keel reduce is positioned and secured. A normal front-loading polyethylene part is then inserted into the tibial tray. The insertion handles ought to diverge about 23 degrees to verify correct alignment of the 2 parts. If it has not been accomplished before, the distractor ought to be removed at this level and the ankle stability examined. Place a three- or four-hole semitubular plate over the lateral aspect of the fibula through the anterior incision. Insert two screws percutaneously via the plate, fibula, and tibia to compress the syndesmosis. Specifically look for and deal with any muscle imbalances (ie, posterior tibial tendon dysfunction). Valgus is usually due to longstanding posterior tibial tendon dysfunction with secondary deltoid ligament instability. Ligamentous varus or valgus of more than 20 degrees may be a contraindication for an ankle substitute with the Agility ankle. Bone erosion varus or valgus with no ligamentous instability is an acceptable indication. Syndesmosis preparation the complete syndesmosis ought to be d�brided before attempting to unfold the fibula from the tibia. Failure to launch the posterior tibiofibular ligament might end in a fibula fracture when spreading the syndesmosis or inserting the tibial component. Locking the foot in plantarflexion will tilt the talar minimize toward the subtalar joint. There is often sufficient bone to insert one or two screws for fixation, or a rigidity band wire method might be used. A leg walker is applied, and the affected person can begin with non�weight-bearing range of movement for 5 minutes thrice a day. At 6 weeks radiographs are obtained, and if there are enough indicators of syndesmosis therapeutic the patient can progress to full weight bearing and begin bodily therapy to improve range of motion, proprioception, and power. Further perioperative issues embody tibial nerve injury, tendon injuries, and wound issues. The use of autologous concentrated progress components to promote syndesmosis fusion in the Agility total ankle replacement: a preliminary study. Total ankle arthroplasty with the Agility prosthesis: scientific and radiographic evaluation. At a mean 9-year follow-up the revision rate was 11% (either a revision or a fusion). Eighty-nine (76%) of the 117 ankles had some evidence of peri-implant radiolucency.
Purchase nicotinell 35 mg free shipping
Peroneal tendon subluxation take a look at: In the susceptible position, with the knee flexed to ninety levels, ankle dorsiflexion and compelled hindfoot eversion towards resistance is carried out. Apprehension and peroneal tendon subluxation or dislocation with this provocative maneuver sometimes confirms the diagnosis. Likewise, continual peroneal tendon subluxation or dislocation might not present with the tendons frankly dislocated. Chronic subluxation and dislocation are generally finest recognized by testing the ankle through a variety of motion of inversion and plantarflexion to most eversion and dorsiflexion with resistance. Successful outcomes of nonoperative administration range from 14% in a research by Eckert and Davis4 to up to 56% as reported by McClennan,9 whereas different investigators have additionally reported variable outcomes in small case sequence. For patients with persistent subluxation, nonoperative therapy has not been shown to assist; often pain and symptoms recur once the short-leg solid is removed. In addition, more athletic, higher-demand sufferers are inclined to demand more reliable therapy and want to proceed with operative restore. The affected person is placed in an oblique lateral position using a beanbag or massive support under the ipsilateral hip. An examination beneath anesthesia with provocative maneuvers such as the anterior drawer and rotary subluxation check might determine associated instability and locking or popping of the unstable peroneal tendons. Preoperative Planning Routine ankle radiographs are important to establish or rule out a rim fracture of the distal fibula, which happens in 15% to 50% of all circumstances of peroneal subluxation. The retinaculum often is lifted off its fibular attachment, thus permitting the peroneal tendons to subluxate. Elevation of an anterior-based periosteal flap (outlined by dots) from the fibular groove has been accomplished. The tendons are relocated, after a groove-deepening process, into the recreated groove. If a shallow or convex fibular groove is present, we usually perform a groove-deepening procedure. After the flap is raised, a groove-deepening procedure could also be performed when indicated. Range the ankle to consider the delicate tissue restore, being positive that the tendons are free to move inside the reconstructed peroneal tendon sheath. Close the skin in traditional trend, and place the leg into acceptable dressings and splints with compressive bandages. Peroneal tendon dislocations predispose the tendons to longitudinal cut up tears because the tendon repeatedly subluxates across the posterolateral fibula. With peroneal tendons reduced, a "new gliding floor" and pocket of displaced superior peroneal retinaculum is clear. Trap door reduced in deepened fibular groove, with impactor getting used to recess the bone and deepen the groove maximally. Peroneal tendons remaining decreased, even with out restore of the superior peroneal retinaculum. If not, then deepen the groove further with a larger-diameter drill bit and carry out further impaction of the posterior fibular surface. With tendons reduced, the pseudogroove is seen, with the displaced and attenuated superior peroneal retinaculum. Using a tamp longitudinally to protect the gliding surface of the posterior fibula throughout its impaction. The flap should keep its continuity, anteriorly, with the fibrocartilage ridge. Flap-to-tendon adhesions Peroneal tendon tears Avoid overtightening the peroneal tendon sheath reconstruction. No points with tendon-to-flap adhesions have been reported; nonetheless, early range of movement starting at four weeks minimizes any chance of adhesions developing. Successful peroneal tendon reduction with persistent symptoms secondary to peroneal tendon tears could result in a poor end result. After four weeks the cast is eliminated and the patient is given a removable stiff-ankle rocker-bottom boot and stays non�weight-bearing for an additional 2 weeks whereas starting bodily therapy with ankle range-of-motion workouts. At the top of 6 weeks the affected person is progressed to weight bearing as tolerated in the brace, after which the affected person is weaned from the stiff-ankle boot and is began with ankle strengthening with inversion and eversion exercises.

French Thyme (Thyme). Nicotinell.
- Are there any interactions with medications?
- How does Thyme work?
- Are there safety concerns?
- Dosing considerations for Thyme.
- Bronchitis, in combination with cowslip; treating hair loss (alopecia areata) when combined with other herbs; improving movement disorders in children when used with other medicines; colic; ear infections; swelling (inflammation) of the tonsils; preventing bedwetting; sore throat; bad breath; bronchitis; and swelling (inflammation) of the lungs and mouth.
- What is Thyme?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96799
Order nicotinell 17.5 mg on line
Before body elimination, small transverse incisions (2 to three cm in length) are made overlying the suitable joints to perform cartilage removing and joint preparation for arthrodesis. Immediately after elimination of the external fixator, a minimally invasive fusion of the midtarsal joint was performed to forestall future Charcot foot collapse. Under fluoroscopic steering, the guidewires for the large-diameter cannulated screws are inserted percutaneously by way of the plantar pores and skin incision into the metatarsal head by dorsiflexing the metatarsophalangeal joint. After the lateral and medial column guidewires (fourth, first, and second metatarsals) are inserted to keep the corrected foot position, the frame is removed and the foot is reprepped. Intramedullary Screw Fixation and Closure Typically, three large-diameter cannulated intramedullary metatarsal screws are inserted: medial and lateral column partially threaded screws for compression of the arthrodesis web site and one central (second metatarsal) totally threaded screw for added stabilization. These screws span the whole size of the metatarsals to the calcaneus and talus, provide compression throughout the minimally invasive arthrodesis web site, and stabilize adjacent joints. The intramedullary metatarsal screws cross an unaffected joint, the Lisfranc joint, thereby protecting the Lisfranc joint from experiencing a future Charcot occasion. The minimally invasive incisions are then closed, and a well-padded L and U splint is utilized. At the time of hospital discharge, the affected person is placed in a non�weight-bearing quick leg forged for two to three months, and then gradual progression to weight bearing is achieved. Note the accurate anatomic discount, fusion of the involved Charcot joint (midtarsal joint), safety of the adjoining Lisfranc joints (stability via screw fixation), ridged inside stability, restoration of foot size, healed ulceration, and preservation of the subtalar and ankle joints. When applying the forefoot 6 6 butt frame, it is necessary to mount the U-plate on the hindfoot as posterior as potential and the forefoot ring as anterior as potential. Bone phase fixation is necessary; otherwise, failure of osteotomy separation or incomplete anatomic reduction occurs. Small wire fixation is most popular in the foot because of the scale and consistency of the bones. When treating a affected person with neuropathy, development of extraordinarily steady constructs is of great significance. External fixation for Charcot deformity correction should embrace a full distal tibial ring with a closed foot ring. When evaluating the average change in preoperative and postoperative radiographic angles, the transverse plane talar�first metatarsal angle, sagittal aircraft talar�first metatarsal angle, and calcaneal pitch angle were all found to be significantly altered. Most notably, no deep an infection, no screw failure, and no recurrent ulcerations occurred and no amputations were needed through the previous 5 years. The advantages of our method compared with the resection and plating technique reported by Schon4 or the resection and exterior fixation method reported by Cooper1 are preservation of foot size (no bone resection), accurate anatomic realignment of soft tissues and bone, and a secure foot. Furthermore, our methodology is much less invasive and permits for partial weight bearing. Application of exterior fixators for management of Charcot deformities of the foot and ankle. Chapter forty six Flexor Digitorum Longus Transfer and Medial Displacement Calcaneal Osteotomy Gregory P. Women are rather more generally affected than men, with a typical age vary older than 50 years. The degree and adaptability of the deformity play a key function in figuring out remedy. The first component of the deformity to turn out to be fixed is usually an elevation of the primary ray relative to the fifth ray. This is the results of a compensation of the forefoot for the hindfoot valgus and known as a onerous and fast forefoot varus. Later, the valgus alignment of the calcaneus by way of the subtalar joint becomes contracted and irreducible. Rarely, a secondary failure of the deltoid ligament alongside the medial side of the hindfoot develops as the mechanical stresses positioned upon it by the flattened arch improve. As the planovalgus deformity develops, the foot collapses via the arch and the Achilles is not stretched to its regular size in a standing or strolling posture. The sag of the arch and the abduction of the forefoot may be described by method of the loss of alignment of the primary metatarsal and the talus. The antagonists to the posterior tibialis are the peroneals, they usually have to be functional for the deformity to develop. Plain foot radiographs must also be examined for the presence of hindfoot arthritis, midfoot arthritis or instability, and an accessory navicular. In some circumstances, lateral impingement develops because the valgus posture of the hindfoot becomes excessive.
Syndromes
- Hunger
- Rapid breathing
- Be able to place objects in mouth
- Trauma
- Nicotine gum (Nicorette)
- Examine the pupils with a penlight to see that they respond (constrict) properly to light.
- The tissue is sent to a lab. There, it is examined under a microscope.
Buy nicotinell 35 mg with mastercard
The semispinalis cervicis arises from the transverse processes of the upper six thoracic vertebrae and inserts onto the spinous processes of C2 to C5. It originates from the articular processes of the decrease cervical vertebrae and inserts onto the spinous processes of the upper cervical vertebrae. They originate from the transverse process of one vertebra and ascend obliquely to insert on the spinous strategy of the vertebra one or two levels cranial to their origin. Osteoligamentous Anatomy the external occipital protuberance or inion is an simply palpable bony landmark in the midportion of the occiput. The superior nuchal line extends as a bony ridge on both facet of this prominence. A small ridge or crest, referred to as the median nuchal line, descends in the medial aircraft from the exterior occipital protuberance to the foramen magnum. The spinous means of the axis is tall, bifid, and broadest within the cervical spine. A broad sheet of thick fibrous tissue called the posterior atlanto-occipital membrane extends from the posterior border of the foramen magnum to the superior border of the posterior arch of the atlas. The posterior atlantoaxial membrane is a broad, thin membrane extending from the inferior border of the posterior arch of the atlas to the superior border of the lamina of the axis. The tectorial membrane is the cranial extension of the posterior longitudinal ligament, running posterior to the transverse ligament to attach onto the anterior border of the foramen magnum. The pars interarticularis or isthmus of C2 is the waist of the posterior arch of C2, connecting the superior and inferior articular processes. The medial margin of the pars interarticularis alongside the superior border of the C2 lamina is a information to the medial margin of the C2 pedicle. The C1�2 side joint is oriented largely within the axial airplane, while the C2�3 and remaining subaxial cervical aspect joints are coronally oriented forty five levels to the airplane of the spine. The C7 spinous course of tends to be straight and lengthy and terminates in a single tubercle. The lateral mass of the cervical backbone refers to the lateral column of every vertebral body that features the superior and inferior articular processes and the transverse foramen on either side. It offers a secure fixation anchor for screw insertion from C3 to C6, notably when the spinous course of and lamina are fractured or eliminated. A faint longitudinal groove marks the separation between the laminae and lateral plenty. The exiting nerve root and posterior portion of the transverse course of lie anterior to the lateral mass. The rectus capitis posterior major originates from the spinous process of the axis and inserts onto the lateral half of the inferior nuchal line. The obliquus capitis superior originates from the transverse strategy of the atlas and inserts onto the occiput laterally between the superior and inferior nuchal traces. The obliquus capitis inferior muscle originates from the spinous means of the axis and inserts onto the transverse means of the atlas. The suboccipital triangle lies between the rectus capitis posterior main and the superior and the inferior obliques. The greater occipital nerve is the medial branch of the posterior division of the second cervical nerve at the medial angle of the suboccipital triangle. It runs cephalad between the semispinalis capitis and the obliquus inferior, towards the occiput, the place it pierces the semispinalis capitis and the trapezius. The suboccipital triangle lies between the rectus capitis posterior main, the obliquus superior, and the obliquus inferior. The higher occipital nerve is seen crossing the suboccipital triangle alongside its medial angle. The posterior arch of the atlas with the vertebral artery is seen within the ground of the suboccipital triangle. Superior, inferior, and median nuchal strains are the distinguished bony ridges on the posterior occipital floor. The major posterior cervical muscles and muscle tissue of the suboccipital triangle insert on these bony ridges and on the posterior occipital floor between these ridges. Sagittal cross-section showing the ligamentous architecture of the proximal cervical spine. Anterior and posterior atlanto-occipital in addition to atlantoaxial ligaments and the ligaments stabilizing the odontoid course of are depicted: the apical ligament of the dens and the transverse ligament of the atlas.
Order nicotinell canada
Baumhauer has demonstrated, via histochemical studies, the cytokines involved with the event of the destructive process, which resembles acute rheumatoid pannus. Trauma, or some unknown inciting issue, initiates a course of that releases specific cytokines. These cytokines lead to the event of destructive grey tissue that histologically resembles rheumatoid pannus. Patients often describe a sense of "crunching" and instability at the involved web site. Eichenholtz8 arbitrarily categorized the timeline of the disease process into three levels. A therapeutic response will usually develop throughout this destructive phase of the disease process, prompting other authors to divide the disease course of into extra stages. This is when the radiographs tackle the attribute appearance of hypertrophic destruction with or without bony repair and the looks of a hypertrophic nonunion. This is the stage when the foot assumes the attribute deformities with hypertrophic reactive bone formation. Eichenholtz8 in 1966 published an in depth monograph based on his observations in 66 sufferers. This goal clinical, radiographic, and histologic information provides goal benchmark information. This monograph objectively describes the destructive illness process as nicely as the progression of deformity. In fact, better than half of sufferers will remember a specific traumatic occasion, although it might be trivial. The first signal of occult an infection within the diabetic is rising blood sugar or growing insulin demand. Patients with deep an infection will typically have an entry portal for infection, which might be so simple as an infected ingrown toenail, or a crack or pinhole between the toes. The erythema often disappears with elevation, in contrast to the patient with a diabetic foot infection. We defined a desired scientific consequence as remaining ulcerfree and sustaining strolling independence with commercially obtainable depth-inlay footwear and custom accommodative foot orthoses. The forged is changed each 14 days until the affected joint is clinically steady and the quantity of the limb stabilizes. Despite shut monitoring, she developed an ulcer within the pores and skin overlying the top of the talus. When multiple surgical attempts failed, a transtibial amputation was necessary because of infection. This patient is clinically plantigrade with sturdy skin and connective tissue aligned for weight-bearing. Despite the deformity, therapy was achieved with a weight-bearing total-contact forged until the acute harmful process subsided. Long-term administration was achieved with commercially available therapeutic footwear (depth-inlay shoes and customized accommodative foot orthoses). Most experts agree that the first step in surgical remedy is a lengthening of the gastrocnemius�soleus motor group to create steadiness between ankle flexors and extensors. Whichever principle one subscribes to , it has turn into apparent that lengthening of the gastrocnemius�Achilles tendon motor unit by gastrocnemius recession or percutaneous Achilles tendon lengthening is essential. Correction of the bony deformity can typically be achieved by eradicating a adequate wedge of bone at the apex of the deformity (ie, a partial tarsectomy) to create a plantigrade foot. Our most well-liked technique of achieving surgical stabilization is with a tension-band three. Despite very careful attention by the affected person and shut monitoring by her physicians, she developed this ulcer using therapeutic footwear 2. This 50-year-old man had repeated lateral foot infections despite resection of the fifth metatarsal. Percutaneous tendon Achilles lengthening was followed by a wedge resection of enough bone, via the ulcer, to appropriate the deformity. Correction of the bony deformity is completed through an incision positioned instantly over or just inferior to the apex of the deformity. A biplanar wedge of bone is resected on the apex of the deformity, permitting correction of the deformity and creation of a plantigrade foot.
Generic nicotinell 35mg overnight delivery
In our palms, symptomatic calcaneocuboid joint arthritis is a sign to carry out the lateral column lengthening via the calcaneocuboid joint and not by way of the anterior means of the calcaneus. Make the incision about 6 to 8 cm long, parallel to the plantar foot, and perpendicular to the calcaneocuboid joint. Place small Hohmann retractors, one within the sinus tarsi and the opposite plantar to the anterior calcaneus, after subperiosteal dissection enhances the exposure to the lateral column. Elevation of the extensor digitorum brevis and retraction of the peroneal tendons with small Hohmann retractors. Osteotomy With a Bovie electrocautery or a marking pen, mark a point on the lateral calcaneus 1. We perform the anterior calcaneal osteotomy with a small oscillating noticed and routinely use irrigation to avoid thermal harm to the bone. Note the open lamina spreader on the back table, to be used as a caliper to measure the bone graft dimension. Measuring the space between the tooth of the lamina spreader for bone graft measurement. Expose the anterior iliac crest using subperiosteal dissection and Taylor retractors. Place the block into the lateral column osteotomy and tamp it in securely with a bone tamp and mallet. We use a small lamina spreader with out tooth and place it in the far dorsal lip of the osteotomy and distract. The allograft comes in simply plantar to that and often can be tamped in with a few taps of the mallet. Occasionally, we temporarily repair the calcaneocuboid joint in its anatomic place with a 0. Undercorrection to residual deformity or overcorrection to an adductus deformity could be avoided by checking for desired alignment with the lamina spreader in place, earlier than sizing and inserting the graft. Identify the peroneal tendons and sural nerve and retract them plantarward, and elevate the extensor digitorum brevis muscle dorsally. Distract the calcaneocuboid joint with a small lamina spreader and take away the articular cartilage from each side of the joint. Distract the calcaneocuboid joint utilizing the small lamina spreader until the specified correction is obtained. Remove the lamina spreader with out altering the quantity of "unfold" on the lamina so it might be used as a caliper to measure the dimensions of the graft. When utilizing allograft, use no less than a 15-mm-wide iliac crest wedge or patellar wedge. Mark the wedge size from the measurement obtained above and then fastidiously cut the block in a "pie" or wedge shape, with the cortical aspect widest. When using autograft, use a regular strategy to the iliac crest, avoiding the superficial department of the femoral nerve, and make an incision about 6 cm long. Mark the scale of the graft from the measurement beforehand obtained and rating the margins with a curved osteotome. Cut the block as a "pie" or wedge in situ, or remove a regular block and trim it to a "pie" or wedge on the back table. Insert the graft within the calcaneocuboid joint, as flush as attainable with the lateral column of the foot, and make sure correction clinically and fluoroscopically. By checking realignment with the lamina spreader earlier than contouring or inserting the graft, overcorrection to adductus deformity and undercorrection with residual abduction is prevented. Watch for the peroneal spastic flatfoot and evaluate appropriately for tarsal coalition. Lateral column lengthening may correct the hindfoot however could worsen the relative forefoot supination. An adjunctive medial column stabilization procedure to plantarflex the first ray could also be necessary (Lapidus procedure or plantarflexion osteotomy of the medial cuneiform). Approach Osteotomy Evaluate and be prepared to treat any concomitant peroneal tendon pathology, such as splits or contracture. Take care not to place the osteotomy too far distal and destabilize the calcaneocuboid joint. Take care to not place the osteotomy too far proximal and violate the center or posterior facet of the subtalar joint. Retract the peroneal tendons with a small Lambotte osteotome beneath the inferior edge of the calcaneus and watch carefully to avoid unintended laceration of the tendons by the oscillating noticed.
References
- Yeo CJ, Cameron JL, Maher MM, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg 1995;222(4):580-592.
- Rosser, J.C. Jr., Young, S.M., Klonsky, J. Telementoring: an application whose time has come. Surg Endosc 2007;21:1458-1463.
- Shen H, Feng C, Jin X, et al. Recurrent exercise- induced acute kidney injury by idiopathic renal hypouricemia with a novel mutation in the SLC2A9 gene and literature review. BMC Pediatr 2014; 14:73.
- Calzolari, E., Bianchi, F., Dolk, H., et al. Omphalocele and gastroschisis in Europe: a survey of 3 million births 1980-1990.
- Moyer RF, Birmingham TB, Bryant DM, et al. Valgus bracing for knee osteoarthritis: a meta- analysis of randomised trials. Arthritis Care Res 2015; 67(4):493-501.
- J Natl Compr Canc Netw. 2015;13:194-227.
- DiNardo CD, Tsai DE. Treatment advances in posttransplant lymphoproliferative disease. Curr Opin Hematol 2010;17:368-374.
- Voss K, Stahl S, Schleider E, et al. CCM3 interacts with CCM2 indicating common pathogenesis for cerebral cavernous malformations. Neurogenetics 2007;8(4):249-56.