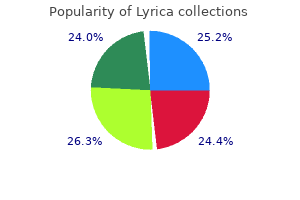
Lyrica dosages: 150 mg, 75 mg
Lyrica packs: 30 pills, 60 pills, 90 pills, 120 pills, 240 pills

Purchase genuine lyrica
Studies in rhesus monkeys have shown that section of the two-third anterior corpus callosum resulted in the development of partial seizures five times faster than in nonbisected animals (9). In the amygdala kindling model of the cat, Wada and Sato (10) 984 Studies in Humans the first series of 10 patients was published in 1940 by Van Wagenen and Herren (1). However, the real interest in this procedure developed almost 30 years later when Wilson reported on the Dartmouth series of callosotomies (14). In general, the clinical series have confirmed the animal studies, demonstrating the efficacy of callosotomy in treating seizures requiring bilateral synchrony for their clinical expression. In contrast, interictal bisynchronous discharges persisted even after a complete section, albeit with a significantly lower frequency. Other authors report a conversion of generalized to partial seizures following callosotomy. The best response has been observed in patients with "drop attacks" presenting as tonic and atonic seizures. In 1996, Phillips and Sakas (29) reported the results of anterior callosotomy in 20 patients. They divided outcome into freedom from seizures and significant reduction (70%) of seizures. Using these criteria, 16 of 20 patients (80%) had significant improvement of at least a 70% decrease in seizure frequency. However, this association of seizure type and ictal electroencephalographic pattern was not predictive of outcome in younger patients (16,30). This view has not been universally accepted; Phillips and Sakas did not find neuroimaging or electroencephalographic findings to be predictive of outcome (29). Patients with complex partial seizures are less likely to respond to this procedure; approximately 40% achieve a significant seizure reduction. Corpus callosotomy had been used in patients with frontal lobe seizures in whom the seizure focus could not be lateralized because of very rapid spread of epileptiform activity. Clark in 2007 found that a planned palliative corpus callosotomy may help identify a resectable epileptic foci (31). Corpus callosotomy may be performed as a partial resection involving the anterior two third (in the majority of cases) or a complete section. Rahimi in 2007 concurred that in patients with secondarily generalized intractable epilepsy complete callosotomy was superior to partial callosotomy (35). Maehara and Shimizu advocate a complete callosotomy, especially in children and in adults with widespread epilepsy (36). In any event, when a complete section is considered, it should be carried out as a two-stage procedure to minimize neuropsychological complications. They found a favorable outcome, defined as a 50% reduction of seizures reported in 60% to 80% of all patients with atonic seizures and tonic seizures resulting in falls. Improvements in quality-of-life indices and social adjustment did not always coincide with reduction in seizure frequency.

Order lyrica 75 mg visa
Non-convulsive status epilepticus in two patients receiving tiagabine add-on treatment. Tiagabine-induced generalised non convulsive status epilepticus in patients with lesional focal epilepsy. Non-convulsive status epilepticus induced by tiagabine in a patient with pseudoseizure. Tiagabine-induced nonconvulsive status epilepticus in an adolescent without epilepsy. Total percentage body weight changes during add-on therapy with tiagabine, carbamazepine and phenytoin. It was first synthesized in the 1950s as a potential tranquilizer, but unlike the related dicarbamate, meprobamate, it has no tranquilizing nor sedative action. An inhibitory effect on high-threshold, voltage-sensitive calcium currents was reported (19). Fluorofelbamate stopped seizures in the rat self-sustaining status epilepticus model; it also retarded the development of subsequent spontaneous seizures, which suggests an antiepileptogenic effect (23). Clearance in children is higher, with mean values 40% higher in children 2 to 12 years old in comparison to adults (30). The "presurgical" design was repeated as a monotherapy trial and further confirmed efficacy (37). Adjunctive open-label use reduced seizure frequency by 53% among 30 children aged 2 to 17 years (38). Atonic seizures (drop attacks) were reduced by 34% and all seizures by 19%, versus a 9% decrease and a 4% increase, respectively, with placebo. The primary endpoint was time to occurrence of the fourth seizure or 29 days, whichever came first. The valproate dose was a compromise between a placebo control, considered unsafe, and a full-dose active control, which could have reduced the chance of detecting a difference (36). It should be noted that 15 mg/kg/day is the recommended starting dose for valproate. Clinically significant interactions with phenytoin, carbamazepine, valproate, and phenobarbital have been established (Table 62. Weight loss is most likely over the first year of use, then weight tends to level off in most patients (57). In one open-label, add-on assessment, behavioral problems were the leading cause of discontinuation (57). The overall dropout rate caused by adverse effects in clinical trials was 12% (33). As expected with most drugs, this rate is higher in community practice-21% in one open-label series (57). Interactions with renally excreted drugs such as levetiracetam, gabapentin, pregabalin, and vigabatrin have not been reported and would not be expected. Doses in the clinical trials were limited to 3600 mg/day for adults and 45 mg/kg/day for children, with most research patients achieving these targets without dose-limiting toxicities. Detailed review of the first 31 cases according to International Agranulocytosis and Aplastic Anemia Study criteria revealed that 23 (74%) met criteria for a diagnosis of aplastic anemia (60). Based on a 1997 estimate of 110,000 patients exposed, the authors of this review suggested a most probable incidence of 127 per million (1/8000 cases), compared with a population rate of 2 per million per year (60). Patients developing aplastic anemia were more likely to have histories of blood dyscrasias, especially cytopenia, autoimmune disorders, and rashes or significant toxicities with previous drugs (62). Caucasian women were the demographic group most likely to develop aplastic anemia (62). Children may be safer; only one child, a postpubescent 14-year-old reported in 2007, has been affected (61). Both felbamate and its initial metabolite, 2-phenyl-1,3-propanediol monocarbamate, cause apoptosis of bone marrow progenitor cells in vitro (67). A Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society has formulated practice guidelines for use in specific patient populations (68) (Table 62. All patients or their caretakers must be able to report side effects reliably, comply with blood testing, and understand the potential risks and benefits. Of these, eight cases could have been caused by other factors-five associated with status epilepticus and one case each of hepatitis A, acetaminophen poisoning, and severe hypotension.
Diseases
- Benign congenital hypotonia
- Hydrocephalus endocardial fibroelastosis cataract
- Michelin tire baby syndrome
- Prostaglandin antenatal infection
- Oral facial digital syndrome type 4
- Exotropia
Discount lyrica 75mg buy
Volatile oils present include low levels of ascaridole, which is toxic: it is Pharmacokinetics No relevant pharmacokinetic data found. Mechanism the mechanism of this apparent interaction remains unknown, and it is not known whether both herbs or just one was responsible for what happened. Both boldo and fenugreek have been reported to contain natural coumarins, but it is unclear whether they have any anticoagulant activity. See natural coumarins, page 297 for more information on the interactions of coumarin-containing herbs. It may be better to advise patients to discuss the use of any herbal products that they wish to try, and to increase monitoring if this is thought advisable. Cases of uneventful use should be reported, as they are as useful as possible cases of adverse effects. Note that the name boneset has also been used for Symphytum officinale (Boraginaceae). Use and indications Boneset is traditionally used for influenza, acute bronchitis and nasopharyngeal catarrh. For information on the pharmacokinetics of individual flavonoids present in boneset, see under flavonoids, page 186. Constituents Sesquiterpene lactones present in the herb include helenalin, euperfolin, euperfolitin, eufoliatin, eufoliatorin and euperfolide. Diterpenes such as dendroidinic acid and hebeclinolide have been reported, as well as the phytosterols sitosterol and stigmasterol, and the flavonoids kaempferol, quercetin, astragalin, hyperoside, rutin and eupatorin. A series of immunostimulatory polysaccharides (mainly 4-O-methylglucuroxylans) have also been described. For information on the interactions of individual flavonoids present in boneset, see under flavonoids, page 186. Not to be confused with other types of frankincense, which are extracted from other Boswellia species and used for their aromatic properties. It was established that cytochrome P450 inhibition occurs irrespective of boswellic acid content, and the constituents responsible for this effect are not removed during the manufacturing of a commercially available product tested in the study (Boswellia serrata extract, H15). Constituents the main active constituents are the boswellic acids, which are lipophilic pentacyclic triterpene acids. The keto derivatives, 11-keto-beta-boswellic acid and acetyl-11-keto-betaboswellic acid, are thought to be particularly potent anti-inflammatory agents. The volatile oils of Boswellia serrata characteristically contain the diterpenes isoincensole and isoincensole acetate. Use and indications Boswellia serrata is used for inflammatory disorders including collagenous colitis (a cause of chronic diarrhoea), peritumoral oedema, rheumatoid arthritis and other chronic conditions. The boswellic acids have immunomodulatory effects and are anti-inflammatory via a number of mechanisms. Interactions overview Some evidence suggests that food may beneficially increase the bioavailability of boswellic acids, but other interaction data are generally lacking. It seems possible that boswellia may interact with conventional drugs by inhibiting P-glycoprotein and/or cytochrome P450 isoenzymes (see Pharmacokinetics, above), but the data are too sparse to make any meaningful predictions. Analysis of frankincense from various Boswellia species with inhibitory activity on human drug metabolising cytochrome P450 enzymes using liquid chromatography mass spectrometry after automated on-line extraction. Pharmacokinetics In an in vitro study, aqueous extracts of Boswellia serrata did not inhibit common cytochrome P450 drug-metabolising enzymes. However, the gum resin was found to have some 81 82 Boswellia Experimental evidence No relevant data found. Importance and management these data show that food intake can significantly increase the bioavailability of boswellic acids, and suggest that Boswellia serrata extracts should be taken with meals, as therapeutic levels may not be achieved when taken on an empty stomach. Effect of food intake on the bioavailability of boswellic acids from a herbal preparation in healthy volunteers. B Boswellia + Food Food appears to beneficially increase the bioavailibility of boswellic acids. Clinical evidence In a crossover study, 12 healthy subjects, after fasting for 10 hours, were given a single 786-mg dose of dry extract (gum resin) of Boswellia serrata (standardised to 55% boswellic acids) with a highfat meal. Constituents Bromelain is a crude, aqueous extract obtained from the pineapple plant, containing a number of proteolytic enzymes.
Lyrica 150mg overnight delivery
Benign partial epilepsy and related conditions: multifactorial pathogenesis with hereditary impairment of brain maturation. Prognosis of benign childhood epilepsy with centrotemporal spikes: a follow-up study of 168 patients. Benign childhood epilepsy with centrotemporal spikes: clinical characteristics and identification of patients at risk for multiple seizures. Partial epilepsy in neurologically normal children: clinical syndromes and prognosis. Status epilepticus in benign rolandic epilepsy manifesting as anterior operculum syndrome. Prolonged intermittent drooling and oromotor dyspraxia in benign childhood epilepsy with centrotemporal spikes. Atypical evolutions of benign partial epilepsy of infancy with centro-temporal spikes. Benign partial epilepsy with centrotemporal (or rolandic) spikes and brain lesion. Abnormal neuroimaging in patients with benign epilepsy with centrotemporal spikes. The course of benign partial epilepsy of childhood with centrotemporal spikes: a meta-analysis. Sulthiame as monotherapy in children with benign childhood epilepsy with centrotemporal spikes: a 6-month randomized, double-blind, placebo-controlled study. Deterioration in cognitive function in children with benign epilepsy of childhood with central temporal spikes treated with sulthiame. Incidence of drug-induced aggravation in benign epilepsy with centrotemporal spikes. Paradoxic reaction to lamotrigine in a child with benign focal epilepsy of childhood with centrotemporal spikes. Benign childhood epileptic syndromes with occipital spikes: new classification proposed by the International League Against Epilepsy. A study of 43 patients with Panayiotopoulos syndrome, a common and benign childhood seizure susceptibility. Panayiotopoulos syndrome: an important electroclinical example of benign childhood system epilepsy. Early onset benign childhood occipital seizure susceptibility syndrome: a syndrome to recognize. Benign childhood focal epilepsies: assessment of established and newly recognized syndromes. Combined myoclonic-astatic and "benign" focal epilepsy of childhood ("atypical benign partial epilepsy of childhood"). Do children with benign rolandic epilepsy have a higher prevalence of migraine than those with other partial epilepsies or nonepilepsy controls Topographic analysis of the centrotemporal discharges in benign rolandic epilepsy of childhood. Benign partial epilepsy of childhood with monomorphic sharp waves in centrotemporal and other locations. Dipole reversal: an ictal feature of benign partial epilepsy with centrotemporal spikes. Dipole reversal: an ictal feature in a patient with benign partial epilepsy of childhood with centro-temporal spike. Neuropsychological findings in children with benign childhood epilepsy with centrotemporal spikes. Neuropsychological disorders related to interictal epileptic discharges during sleep in benign epilepsy of childhood with centrotemporal or rolandic spikes. High risk fo reading disability and speech sound disorder in rolandic epilepsy families: case-control study.

Buy lyrica overnight
Levetiracetam inhibits the high-voltage-activated Ca (2) current in pyramidal neurones of rat hippocampal slices. In vitro evaluation of potential drug interactions with levetiracetam, a new antiepileptic agent. Effects of antiepileptic comedication on levetiracetam pharmacokinetics: a pooled analysis of data from randomized adjunctive therapy trials. Levetiracetam does not alter the pharmacokinetics of an oral contraceptive in healthy women. Repeated administration of the novel antiepileptic agent levetiracetam does not alter digoxin pharmacokinetics and pharmacodynamics in healthy volunteers. Lack of effect of repeated administration of levetiracetam on the pharmacodynamic and pharmacokinetic profiles of warfarin. Effect of levetiracetam on the pharmacokinetics of adjunctive antiepileptic drugs: a pooled analysis of data from randomized clinical trials. Levetiracetam for partial seizures: results of a double-blind, randomized clinical trial. Multicenter double-blind, randomized, placebo-controlled trial of levetiracetam as add-on therapy in patients with refractory partial seizures. Efficacy and tolerability of levetiracetam 3000 mg/d in patients with refractory partial seizures; a multicenter, double-blind, responder-selected study evaluating monotherapy. An open-label study of levetiracetam at individualised doses between 1000 and 3000 mg day (1) in adult patients with refractory epilepsy. Efficacy and tolerability of levetiracetam during 1-year follow-up in patients with refractory epilepsy. A multicentre, double-blind, randomized parallel group study to evaluate the tolerability and efficacy of two oral doses of levetiracetam, 2000 mg daily and 4000 mg daily, without titration in patients with refractory epilepsy. Clinical experience of marketed levetiracetam in an epilepsy clinic-a one year follow up study. Comparison of levetiracetam and controlled-release carbamazepine in newly diagnosed epilepsy. Levetiracetam versus carbamazepine monotherapy for partial epilepsy in children less than 16 years of age. Efficacy and safety of levetiracetam in children with partial seizures: an open-label trial. Once daily extended release levetiracetam as adjunctive treatment of partial-onset seizures in patients with epilepsy; a double blind, randomized, placebo-controlled trial. Levetiracetam intravenous infusion as alternative to oral dosing in patients with partial-onset seizures. Levetiracetam intravenous infusion: a randomized, placebo-controlled safety and pharmacokinetic study. Single dose bioavailability of levetiracetam intravenous infusion relative to oral tablets and multiple dose pharmacokinetics and tolerability of levetiracetam intravenous infusion compared with placebo in healthy subjects. Double-blind placebo-controlled trial of adjunctive levetiracetam in pediatric partial seizures. Maximum serum concentrations are attained within 45 to 90 minutes in the fasting state and after a mean of 2. The E- and Z-5-oxo-tiagabine isomers are the prominent metabolites in plasma and urine. Similarly, twice-daily and thrice-daily regimens for patients with partial epilepsy were equally effective both during titration to 40 mg/day and a flexible continuation period of 12 weeks at 30 to 70 mg/day. However, the half-life of the agent is increased to 12 to 16 hours in patients with hepatic impairment (35), necessitating dosage reductions and less frequent dosing intervals. A meta-analysis of the five placebo-controlled studies found a relative risk of 3.

Lyrica 75mg order otc
The only statistically different finding was the time for regaining consciousness in children that presented unconscious to the emergency department, for valproate 58. Summary: the evidence finds no difference between phenytoin and valproic acid in the setting of partial and generalized epilepsy (excluding myoclonus and absence seizures) in adults and children for a variety of outcome measures. No difference was found between intravenous valproate or phenytoin in an emergency room setting of children with acute motor focal or generalized seizures, although unconscious children regained consciousness significantly more rapidly with valproate. Phenytoin vs Carbamazepine A Cochrane Review117 compared phenytoin and carbamazepine monotherapy for the treatment of partial onset or generalized seizures in children and adults. A total of 12 trials were identified, of which 4 trials (N=595) included individual participant data and were included in the review. Trials were of overall good quality although the authors suggest that up to 30% of patients may have had their seizure type misclassified. Outcome measures included time to 6-month remission, time to 12-month remission, time to first seizure post randomization and time to treatment withdrawal as a measure of tolerability. No significant difference was found in any outcome measure between phenytoin and carbamazepine including serious adverse events. Adverse events reflected the product labeling with no serious or unusual events noted. Summary: Limited evidence which may be confounded by misclassified seizure type, finds no difference in efficacy between phenytoin and carbamazepine for 58 efficacy measures in children and adults with partial onset or generalized seizures. Carbamazepine use resulted in a higher discontinuation rate, suggesting lower tolerability. Phenobarbitone/Phenobarbital vs Phenytoin A Cochrane Review118 compared phenobarbitone vs phenytoin for monotherapy treatment of generalized, tonic-clonic seizures or partial onset seizures in adults of children. Individualized participant data was found in 4 of 8 identified trials for 599 participants reflecting 63% of the data. Care must be taken when interpreting the skewed data with 78% of participants having partial onset seizures and 22% generalized seizures. For every measure of time to treatment withdrawal (pooled participants, pooled by seizure type or stratified by seizure type) phenobarbitone treatment resulted in statistically more withdrawals than phenytoin. The time to 6- and 12-month remission did not differ between the two groups, however, summary statistics with wide confidence intervals do not support equivalence. The time to the first, post-randomization seizure did not differ between treatment groups. Overall, no difference in seizure control was identified between phenobarbitone and phenytoin although phenytoin therapy resulted in significantly fewer treatment withdrawals which may reflect better tolerability. Painter et al119 compared phenobarbital and phenytoin when dosed to predetermined serum concentrations in 59 neonates with seizures. Combination therapy resulted in similar results regardless of whether the patient received phenobarbital or phenytoin initially (57% vs 62%, respectively; p=0. Summary: the evidence suggests that phenobarbitone and phenytoin are not different in efficacy outcomes for neonatal seizures. Although response rates were not statistically different, the evidence is insufficient to prove equivalence in the treatment of generalized, tonic-clonic and partial seizures in adults and children with phenytoin better tolerated. Carbamazepine vs Valproate Marson et al120 performed a meta-analysis comparing valproate and carbamazepine therapy in the treatment of epilepsy in children and adults in which a misdiagnosis of epilepsy could not be ruled out. Assessed outcomes included the retention time, time to first post-randomization seizures and time to 12-month remission. In the setting of generalized-onset seizures no difference was found between treatments. Summary: Evidence, which may be confounded by misclassified seizure type, finds both carbamazepine and valproate were equally efficacious in the treatment of generalized and partial-onset epilepsy in adults and children. Methsuximide 59 Methsuximide was prospectively studied in an open-label protocol of 112 children with epilepsy refractory to first line antiepileptic drugs or combinations or antiepileptic drugs. Methsuximide serum concentrations were positively correlated with reversible ataxia and leukopenia when >45 mg/L. Tennison et al122 found methsuximide efficacious when added to the current regiment of children with intractable epilepsy on maximal, combination therapy. A reduction in seizure frequency was achieved in >50% of children and was maintained for a mean of 19 months although no patient achieved complete seizure remission.
Lysimachia nummularia (Moneywort). Lyrica.
- What is Moneywort?
- Skin problems such as eczema, killing bacteria, diarrhea, increasing saliva, cough, and other conditions.
- Dosing considerations for Moneywort.
- Are there safety concerns?
- How does Moneywort work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96092

Generic lyrica 150mg overnight delivery
The patient was drinking almost 2 litres of cranberry juice daily, because of recurrent urinary tract infections, and was advised to stop drinking this. The cranberry concentrate had no effect on platelet aggregation, and had no effect on the pharmacokinetics of either R- or S-warfarin. Importance and management Evidence appears to be limited to two experimental studies. Taken on its own, this evidence suggests the possibility of a modest interaction, and therefore some caution might be warranted in patients taking nifedipine who drink cranberry juice. C Cranberry + Tizanidine Limited evidence suggests that cranberry juice does not appear to affect the pharmacokinetics of tizanidine. Clinical evidence In a randomised, crossover study in 10 healthy subjects 200 mL of cranberry juice three times daily for 10 days had no significant effect on the pharmacokinetics of a single 1-mg oral dose of tizanidine taken on day 5. In this study, the cranberry juice used was a concentrate (Kontiomehu sokeroitu karpalomehu) diluted 1 to 4 with tap water before use. Importance and management Although the evidence is limited to this particular study, there appears to be no need for any special precautions when taking cranberry juice with tizanidine. For example, the salicylate constituent of commercial cranberry juice might cause hypoprothrombinaemia. Controlled studies have not found a pharmacokinetic interaction, and only one of four studies found any evidence for an increase in warfarin effect. This might be explained if the interaction is dose dependent (in one of the cases where cranberry intake was mentioned a quantity of 2 litres daily was being consumed), or if it is product dependent. However, it could also be that there is no specific interaction, and that the case reports just represent idiosyncratic reactions in which other unknown factors. Committee on Safety of Medicines/Medicines and Healthcare products Regulatory Agency Possible interaction between warfarin and cranberry juice. Committee on Safety of Medicines/Medicines and Healthcare products Regulatory Agency Interaction between warfarin and cranberry juice: new advice. Warfarin-cranberry juice interaction resulting in profound hypoprothrombinemia and bleeding. A randomized, double-blind trial of the interaction between cranberry juice and warfarin. Pharmacodynamic interaction of warfarin with cranberry but not with garlic in healthy subjects. Interaction of flurbiprofen with cranberry juice, grape juice, tea, and fluconazole: in vitro and clinical studies. C Creatine N-(Aminoiminomethyl)-N-methylglycine C Types, sources and related compounds Creatine monohydrate. Use and indications Creatine supplements are taken most often to improve exercise performance and increase muscle mass. Creatine is found in foods, most abundantly in meat and fish, and is also synthesised endogenously. Excessive intake of creatine, by the use of supplements, has, very rarely, been reported to cause acute renal impairment. The maximum plasma level of creatine is reached less than 2 hours after the ingestion of doses of under 10 g, but after more than 3 hours for doses over 10 g, and may vary with the ingestion of carbohydrate, see food, page 157. Clearance of creatine would appear to be dependent on both skeletal muscle and renal function. There is an isolated report of stroke in a patient taking a creatine supplement with caffeine plus ephedra, although the role of creatine in this case is uncertain. There is a possibility that creatine supplements might complicate interpretation of serum creatinine measurement. Pharmacokinetics Creatine is distributed throughout the body, with the majority being found in skeletal muscle. Creatine is degraded to creatinine, and both creatine and creatinine are excreted via the kidneys. Absorption of creatine is likely to be an active process, and may follow nonlinear kinetics with the 156 Creatine 157 Creatine + Caffeine Limited evidence suggests that the performance-enhancing effects of creatine may be reduced by caffeine. Clinical evidence Nine healthy subjects given a creatine supplement 500 mg/kg daily for 6 days, and caffeine capsules 5 mg/kg daily for 3 days beginning on the fourth day, experienced a lack of performance-enhancing effects of creatine during knee extension exercises, when compared with creatine given alone. Caffeine 5 mg/kg reduced phosphocreatine resynthesis during rest from a period of exercise when given with creatine 25 g daily for 2 or 5 days. Importance and management these studies are preliminary and there seem to be no further reports of an interaction.
Order 150mg lyrica with mastercard
The old classification would have called these unclassified or unofficially, myoclonic-astatic seizures. A 35 year-old man with juvenile myoclonic epilepsy has seizures beginning with a few bilateral arm jerks, followed by stiffening of all limbs and then rhythmic jerking of all limbs. Examples Old = myoclonic seizures followed by a tonic-clonic seizure New = myoclonic-tonic-clonic seizures 8. A 35 year-old man with juvenile myoclonic epilepsy has seizures beginning with a few regularly-spaced jerks, followed by stiffening of all limbs and then rhythmic jerking of all limbs. No corresponding single seizure type existed in the old classification, but they might have been called myoclonic seizures followed by a tonic-clonic seizure. A 14-month old girl has sudden flexion of both arms with head flexing forward for about 2 seconds. Examples Old = infantile spasms (focality not specified) New = focal epileptic spasms 9. A 14-month old girl has sudden flexion of both arms with head flexing forward for about 2 seconds. Because of the ancillary information, the seizure type would be considered to be focal epileptic spasms (the term "motor" can be assumed). The previous classification would have called them infantile spasms, with information on focality not included. There is an approximately 7% incidence of de novo psychosis following temporal lobectomy for epilepsy that tends to occur within the first year following surgery [60]. Post-surgical psychosis may be more likely to occur in those with early onset epilepsy and abnormal pre-morbid personality traits [61]. Some studies have suggested a preponderance of right-sided temporal lobe surgeries among patients with post-surgical psychosis, but this has not been supported by later studies [60]. This study examined reasons for drug discontinuation and may not reflect psychotic episodes that did not precipitate discontinuation of the drug (for example if the episodes were not attributed to levetiracetam). Drug-induced psychosis should be considered whenever psychosis emerges immediately after the addition of a drug to which the patient is naive. Ultimately, though, many of these episodic psychoses may be multifactorial and difficult to place in a particular category. Similarly, patients with a past history of psychosis are more likely to develop psychosis with new drugs [59]. Thus, specific situational factors such as a limbic seizures or specific drugs may contribute to the development of a psychotic state, either in isolation or in combination, in certain patients who are susceptible because of pre-existing structural or genetic factors. When psychosis and epilepsy occur together in the same patient, a neurologic cause common to both must be sought, particularly when the psychosis precedes the onset of epilepsy. Pathology of the temporal lobes has a tendency to cause both epilepsy and psychosis [63]. Traumatic brain injury may significantly increase the risk for both psychosis and epilepsy, particularly when the temporal lobes are affected. Similarly, tumors involving the temporal lobes may cause both seizures and psychosis. Stimulant drugs such as cocaine or amphetamines may trigger both psychosis and seizures, particularly in susceptible individuals [64-67]. Withdrawal from benzodiazepines and alcohol can also trigger seizures as well as psychosis. However, from time to time, an undiagnosed seizure disorder may be suspected in a patient with new onset psychosis, particularly when the nature of the psychotic presentation is atypical for a primary psychiatric disorder. When new psychiatric symptoms appear, the psychiatrist is tasked with evaluating and excluding a psychosis secondary to a medical condition before a primary psychiatric disorder can be diagnosed [23]. A careful history must be obtained to assess for convulsive seizures or recurrent discrete episodes of alteration of awareness or loss of consciousness, particularly when there is a clear onset and offset and a return to normal mental status in between. Collateral history is often necessary, as psychotic patients may be unreliable historians. Seizures may occasionally be misdiagnosed as thought blocking, catatonia, or responding to internal stimuli, if a clinician assumes a primary psychotic disorder and does not consider alternative possibilities. Seizures should be considered if a patient has a known neurological disorder associated with epilepsy, and if the psychotic symptoms are associated with prominent confusion or other neurological signs. Seizures may also be considered in the differential for recurrent brief psychotic episodes with return to baseline in between [71].
Generic lyrica 75mg amex
Other data showed numerically more patients discharged from the hospital in the 5-day group than in the 10-day group (60% vs. Also, although patients were randomly assigned on a 1:1 basis, those assigned to the 10-day group had significantly worse clinical status at baseline (p = 0. Administration Information General Administration Information For storage information, see the specific product information within the study protocols. The significant known and potential risks and benefits of remdesivir, and the extent to which such risks and benefits are unknown. Information on available alternative treatments and the risks and benefits of those alternatives. If providing this information will delay treatment to a degree that would endanger the lives of patients, the information must be provided to the patients as soon as practicable after remdesivir is administered. Intravenous Administration If the patient is enrolled in a clinical trial, follow the specific instructions provided by the study protocol. Lyophilized Powder Reconstitution: **For pediatric patients weighing less than 40 kg, use only the lyophilized powder formulation to prepare doses. For each 100 mg vial, reconstitute with 19 mL of Sterile Water for Injection to give a concentration of 5 mg/mL. Discard the vial if vacuum does not pull the Sterile Water for Injection into the vial. If the contents of the vial are not completely dissolved, shake for another 30 seconds and then allow to settle for 2 to 3 minutes. Repeat this process as needed until the contents are fully dissolved, resulting in a clear solution. Storage: Store remdesivir lyophilized powder vials below 30 degrees C (below 86 degrees F) until required for use. Total storage time from reconstitution to administration should not exceed 4 hours at room temperature (20 to 25 degrees C; 68 to 77 degrees F) or 24 hours under refrigeration (2 to 8 degrees C; 36 to 46 degrees F). Injection Solution: **Do not use to prepare doses for pediatric patients weighing less than 40 kg. Remove remdesivir injection solution from refrigerator and allow to come to room temperature (20 to 25 degrees C; 68 to 77 degrees F) before diluting. Inspect vial to ensure container closure is free from defects, and the solution is free of particulate matter before use. Storage: Store remdesivir injection solution under refrigeration (2 to 8 degrees C; 36 to 46 degrees F) until required for use. If using remdesivir injection solution (not reconstituted powder), inject approximately 10 mL of air into the remdesivir vial above the solution level before withdrawing dose to facilitate withdrawal. Storage: the prepared solution is stable for 4 hours at room temperature (20 to 25 degrees C; 68 to 77 degrees F) or 24 hours under refrigeration (2 to 8 degrees C; 36 to 46 degrees F). If prepared using reconstituted lyophilized powder, total storage time from reconstitution to administration should not exceed 4 hours at room temperature or 24 hours under refrigeration. Storage: the prepared solution is stable for 4 hours at room temperature (20 to 25 degrees C; 68 to 77 degrees F) or 24 hours under refrigeration (2 to 8 degrees C; 36 to 46 degrees F). If prepared using reconstituted lyophilized powder, total storage time from reconstitution to administration should not exceed 4 hours at room temperature or 24 hours under refrigeration. Dilution for Pediatric Loading Dose (patients weighing less than 40 kg): Use only the reconstituted lyophilized powder formulation. Storage: the prepared solution is stable for 4 hours at room temperature (20 to 25 degrees C; 68 to 77 degrees F) or 24 hours under refrigeration (2 to 8 degrees C; 36 to 46 degrees F). For solutions prepared using the reconstituted lyophilized powder, total storage time from reconstitution to administration should not exceed 4 hours at room temperature or 24 hours under refrigeration. Dilution for Pediatric Maintenance Doses (patients weighing less than 40 kg): Use only the reconstituted lyophilized powder formulation. Storage: the prepared solution is stable for 4 hours at room temperature (20 to 25 degrees C; 68 to 77 degrees F) or 24 hours under refrigeration (2 to 8 degrees C; 36 to 46 degrees F).
Order lyrica no prescription
Information obtained by functional mapping can be used to direct surgery and cortical mapping necessary for anatomic confirmation and resection. Focal physiological uncoupling of cerebral blood flow and oxidative metabolism during somatosensory stimulation of human subjects. Dynamic magnetic resonance imaging of human brain activity during primary sensory stimulation. Preoperative mapping of the supplementary motor area in patients harboring tumors in the medial frontal lobe. Effects of anomalous language representation on neuropsychological performance in temporal lobe epilepsy. Most importantly, studies can be repeated to confirm findings, especially if no or unusual activation patterns are found. A number of different paradigms can be performed to map different aspects of language and speech-often more than can be performed in the operating room. To be studied successfully, patients must be awake and cooperative and must lie still. Motion artifact remains the principal cause of failed studies, a particular issue in very young, fidgety, or cognitively impaired patients (though older cognitively impaired patients may do quite well). Activation is task and control specific; a given task may not be optimal for identifying targeted cortex. The role of early left-brain injury in determining lateralization of cerebral speech functions. Utility of preoperative functional magnetic resonance imaging for identifying language cortices in patients with vascular malformations. Use of preoperative functional neuroimaging to predict language deficits from epilepsy surgery. Brain mapping in sedated infants and young children with passive-functional magnetic resonance imaging. Left hippocampal pathology is associated with atypical language lateralization in patients with focal epilepsy. Is language lateralization in temporal lobe epilepsy patients related to the nature of the epileptogenic lesion Limitations to plasticity of language network reorganization in localization related epilepsy. Distinct right frontal lobe activation in language processing following left hemisphere injury. Dissociating the human language pathways with high angular resolution diffusion fiber tractography. Hemispheric specialization in human dorsal frontal cortex and medial temporal lobe for verbal and nonverbal memory encoding. Side of seizure focus predicts left medial temporal lobe activation during verbal encoding. New developments in noninvasive mapping procedures have since further limited its use, although some indications may remain. Paradigm variations primarily involve the procedure, stimulus presentation, and testing methodology (4). The anesthetic drug most commonly used is a barbiturate, either amobarbital or methohexital. The initial step consists of completion of a cerebral angiogram via the transfemoral route to assess cerebral vasculature and cross-filling from one hemisphere to the other. Immediately after the angiogram, the catheter is moved into the internal carotid artery, and the location of the catheter is confirmed on fluoroscopy. Prior to barbiturate injection, the patient is instructed to lift both hands in the air and to start counting. If the injected hemisphere is dominant for language, the patient may stop counting.
Real Experiences: Customer Reviews on Lyrica
Onatas, 65 years: Government Accountability Office, Bureau of Indian Affairs and Indian Health Service Need Great Insight into Implementation at Regional Offices (July 2015), 19. Immediate-release tablets are given 2 to 3 times per day and the suspension is given 4 times per day.
Rufus, 46 years: The teratogenicity of hydantoins and barbiturates in humans, with considerations on the etiology of malformations and cerebral disturbances in the children of epileptic parents. Linear sebaceous nevi are a family of disorders with distinctive raised, waxy, sometimes verrucous nevi on the scalp or face, associated with hemihypertrophy, hemimegalencephaly, and neonatal seizures (142).
Emet, 29 years: Together, these people cost 157 years of life, suggesting that they were on average over the age of 70. Population analysis of the dose-dependent pharmacokinetics of zonisamide in epileptic patients.
Lee, 49 years: Note that ashwagandha has also been known as Indian ginseng, which should not be confused with the common ginsengs, page 219. After a 3-month prospective baseline, subjects were randomized to placebo, Prempro (0.
9 of 10 - Review by J. Marus
Votes: 152 votes
Total customer reviews: 152
References
- Lesnik Oberstein SA, van den Boom R, van Buchem MA, et al. Cerebral microbleeds in CADASIL. Neurology 2001;57(6): 1066-70.
- Hashizume T, Komatsu H, Ishihara S, et al. Pulmonary blastoma in National Sanatoria. Haigan 1997; 37:427-32.
- Barnett v. Bachrach: 34 A.2d 626; 1943.
- Lee BH, Hecht JL, Pinkus JL, Pinkus GS. WT1, estrogen receptor, and progesterone receptor as markers for breast or ovarian primary sites in metastatic adenocarcinoma to body fluids. Am J Clin Pathol 2002; 117(5):745-50.
- Wei W- H, Guo Y, Kindt AS, et al. Abundant local interactions in the 4p16.
- Kurose K, Ohue Y, Wada H, et al. Phase Ia study of FoxP3+ CD4 Treg depletion by infusion of a humanized anti- CCR4 antibody, KW-0761, in cancer patients. Clin Cancer Res 2015;21(19):4327-4336.
- Neuberger A, Rimington C, Wilson JMG. Studies on alcaptonuria II. Investigations on a case of human alcaptonuria. Biochem J 1947;41:438.
- Schnall MD, Pollack HM: Magnetic resonance imaging of the prostate gland, Urol Radiol 12(2):109n114, 1990.

