Glyset dosages: 50 mg
Glyset packs: 30 pills, 60 pills, 90 pills

Discount glyset 50mg
Differences in enhancement patterns between benign and malignant liver lesions have been well reported and are mentioned in individual entities later. These hepatobiliary particular distinction brokers are taken up to varying levels by functioning hepatocellular tissue and are excreted in bile as well as through the kidneys. These distinction brokers are all administered intravenously, although the dose and pharmacokinetics are completely different. These brokers provide comprehensive details about the hepatic parenchyma, bile ducts, and liver vasculature (Burke et al, 2013; Seale et al, 2009). Precontrast and postcontrast T1-weighted imaging is also performed to assess enhancement patterns of the liver parenchyma and liver lesions. If a hepatobiliary distinction agent is used, extra delayed hepatobiliary phase photographs are acquired. Using fast gradient-echo techniques, fats and water protons that share the identical voxel might be imaged both "in section" or a hundred and eighty levels "out of phase. Areas of fatty sparing will stay hyperintense relative to the encircling fatty liver on out-of-phase imaging. The appearance on T2-weighted pictures depends on the sort of sequence acquired and whether or not fat saturation is used. C, T1-weighted out-of-phase image reveals geographic areas (arrow) which have lost sign. Newer, breath-hold three-dimensional (3D) T1 techniques with interpolation allow quick single breath-hold acquisition with added fat and water separation (Bashir et al, 2012). Enhancement characteristics also help within the analysis, as focal fatty liver enhancement ought to parallel surrounding normal hepatic parenchyma. Cysts preserve their markedly high signal on heavily T2-weighted pictures, much like fluid within the cerebrospinal fluid, bile ducts, and pancreatic duct. Iron Deposition Disease Hepatic iron deposition may happen from primary genetic hemochromatosis or from secondary nongenetic systemic overload (see Chapter 76). Primary hemochromatosis is an autosomal recessive genetic disorder characterised by irregular intestinal iron absorption, with accumulation of iron in the nonreticuloendothelial organ system. This predominantly occurs in hepatocytes later within the illness when different viscera, together with the pancreas and coronary heart, are more probably to be concerned. The liver reveals abnormally low sign intensity compared with spleen on T1-weighted in-phase sequences. T1-weighted gradient-echo sequences are very delicate for detecting the presence of iron inside the hepatic parenchyma due to the native area inhomogeneities caused by the presence of iron. Nongenetic systemic iron overload from secondary causes can generally be distinguished from major hemochromatosis based mostly on the pattern of organ involvement. Hemangioma Hepatic hemangiomas (see Chapter 90A) are benign tumors of the liver with an estimated incidence of 20% (Albiin, 2012). On T1-weighted images, hemangiomas are hypointense compared with the encompassing hepatic parenchyma, have clean, well-marginated borders, and are frequently lobulated. Hemangiomas are markedly hyperintense in contrast with normal liver on T2-weighted images. Hemangiomas also are probably to retain a excessive signal on extra closely T2-weighted sequences, nearly to the same degree as cysts, and turn out to be more conspicuous in contrast with surrounding liver parenchyma. Larger hemangiomas are inclined to follow these criteria extra frequently, though large hemangiomas also could have variable sign depth and a central scar (Prasanna et al, 2010). Problems arise with smaller hemangiomas, nevertheless, which may "flash fill" and appear as hypervascular, homogeneous lesions. These smaller lesions (usually <1 cm) may be distinguished by both their T2 sign characteristics and enhancement sample paralleling enhancing vessels (Albiin, 2012). Caution should be used when assessing enhancement using the hepatobiliary contrast agent gadoxetate disodium, nevertheless, as the overlapping extracellular part and hepatobiliary excretion of this distinction could confound the everyday hemangioma enhancement and result in "pseudowashout" in late dynamic part, making characterization harder (Goshima et al, 2010). Sclerosed hemangiomas symbolize a diagnostic problem, usually mimicking malignancies in the liver; restricted knowledge recommend that growing sclerosis shows corresponding decreased T2 sign and less avid enhancement, in all probability corresponding to areas of fibrosis. We will focus on frequent benign and malignant liver lesions and emphasize distinguishing imaging characteristics.

Purchase 50 mg glyset with amex
Readmission for gallstone related issues (pancreatitis, cholecystitis, cholangitis, jaundice, colic) were significantly more widespread in the interval group than the same-admission group (17% vs. These results remained vital when evaluating sufferers with endoscopic sphincterotomy in a subgroup evaluation. As with the earlier retrospective studies, there was no difference in size of keep, A. Gallstones and Gallbladder Chapter 36C Stones in the bile duct: endoscopic and percutaneous approaches 621 problem of surgical procedure, conversions from laparoscopic to open surgical procedure, or well being care use between the two groups. Usually a delay in surgery in these sufferers is secondary to critical illness or while awaiting different surgical or endoscopic treatments for complications similar to a cyst-gastrostomy for a pseudocyst or debridement of walled-off pancreatic necrosis. In the acute setting, an endoscopic strategy to biliary pancreatitis presents the theoretical benefit of instant aid of ampullary obstruction and ductal clearance with out the risks of surgery. Patients with gentle pancreatitis had comparable outcomes no matter treatment strategy. Overall, no important variations have been found in the incidences of both local (10. Patients with biliary obstruction and cholangitis were additionally included in this examine. The remaining 205 patients were randomized to conventional remedy or sphincterotomy regardless of the cholangiographic findings. Compared with standard remedy, the authors showed a major advantage for sufferers handled endoscopically with respect to morbidity (17% vs. The overall mortality and complication rates had been comparable between the two groups regardless of the severity of pancreatitis, however the rate of serious respiratory failure was higher within the invasive group (P =. A current metaanalysis of the seven known well-designed, randomized, managed trials on this matter confirms these identical findings (Uy et al, 2009). Endoscopic techniques are properly established, and equipment have been developed to enhance success and security. Advancement in endoscopic techniques allows the management of complicated bile duct stone illness. Patients with acute cholangitis ought to be considered for pressing endoscopic management. Integrated endoscopic therapy for biliary disease is well established in facilities the place surgeons and endoscopists work closely together and supply one another with an acceptable discussion board for critical analysis of different therapeutic strategies. Gallstones and Gallbladder Chapter 36C Stones within the bile duct: endoscopic and percutaneous approaches 622. Das A, et al: Treatment of biliary calculi using holmium:yttrium aluminium garnet laser, Gastrointest Endosc forty eight:207�209, 1998. Deviere J, et al: Successful management of benign biliary strictures with totally coated self-expanding steel stents, Gastroenterology 147:385� 395, 2014. Diaz D, et al: Methyl tert-butyl ether in the endoscopic remedy of widespread bile duct radiolucent stones in elderly sufferers with nasobiliary tube, Dig Dis Sci 37:97�100, 1992. DiSario J, et al: Biliary and pancreatic lithotripsy devices, Gastrointest Endosc sixty five:750�756, 2007. Ersoz G, et al: Biliary sphincterotomy plus dilation with a large balloon for bile duct stones which may be tough to extract, Gastrointest Endosc fifty seven:156�159, 2003. Escourrou J, et al: Early and late complications after endoscopic sphincterotomy for biliary lithiasis, with and without the gallbladder "in situ. The German Study Group on Acute Biliary Pancreatitis, N Engl J Med 336:237�242, 1997. Garcia-Cano J, et al: Fully coated self-expanding metallic stents within the administration of inauspicious common bile duct stones, Rev Esp Enferm Dig one hundred and five:7�12, 2013. Akcakaya A, et al: Mechanical lithotripsy and/or stenting in administration of difficult widespread bile duct stones, Hepatobiliary Pancreat Dis Int eight:524�528, 2009. Arya N, et al: Electrohydraulic lithotripsy in 111 sufferers: a protected and effective therapy for tough bile duct stones, Am J Gastroenterol 99:2330�2334, 2004. Bhandari S, et al: Usefulness of single-operator cholangioscope-guided laser lithotripsy in patients with Mirizzi syndrome and cystic duct stones: experience at a tertiary care center, Gastrointest Endosc 2016; Jan 5 [Epub forward of print].
Buy glyset visa
They have an incidence of infectious morbidity and 3-month mortality rates twice that of well-nourished sufferers present process liver transplant (Harrison et al, 1997). Pretransplant nutritional standing and illness severity are independently associated with infectious episodes throughout hospitalization (Meril et al, 2009). Nutritional dietary supplements, together with vitamins, should be taken in an effort to attenuate additional nutritional deficits and to replenish losses. Increasing proof exhibits that particular nutrients administered under specific situations to choose patients can modulate metabolic occasions in patients with hepatobiliary disease undergoing operation. Armbrecht U: Chronic pancreatitis: weight reduction and poor bodily performance�experience from a specialised rehabilitation centre, Rehabilitation (Stuttg) 40:332�336, 2001. Astarcioglu I, et al: High levels of glycogen within the donor liver improve survival after liver transplantation in rats, Transplant Proc 23:2465� 2466, 1991. Bachmann J, et al: Cachexia worsens prognosis in sufferers with resectable pancreatic most cancers, J Gastrointest Surg 12(7):1193�1201, 2008. Balzano G, et al: Fast-track restoration programme after pancreaticoduodenectomy reduces delayed gastric emptying, Br J Surg 95(11): 1387�1393, 2008. Bartels M, et al: Pilot research on the effect of parenteral vitamin E on ischemia and reperfusion-induced liver injury: a double-blind, randomized, placebo-controlled trial, Clin Nutr 23(6):1360�1370, 2004. Bauer M, Kiehntopf M: Shades of yellow: monitoring nutritional wants and hepatobiliary function within the critically unwell, Hepatology 60(1):26� 29, 2014. Bell H, et al: Reduced focus of hepatic alpha tocopherol in patients with alcoholic liver cirrhosis, Alcohol Alcohol 27:39�46, 1992. Bengmark S: Nutrition of the critically ill-emphasis on liver and pancreas, Hepatobiliary Surg Nutr 1(1):25�52, 2012. Bianchi G, et al: Update on branched-chain amino acid supplementation in liver ailments, Curr Opin Gastroenterol 21:19�20, 2005. Billiar T, et al: Fatty acid intake and Kupffer cell function: fish oil alters eicosanoid and monokine production to endotoxin stimulation, Surgery 104:343�349, 1988. Birlouez-Aragon I, et al: Antioxidant nutritional vitamins and degenerative pathologies: a evaluation of vitamin C, J Nutr Health Aging 7:103�109, 2003. Braga M, et al: Oral preoperative antioxidants in pancreatic surgery: a double-blind, randomized, scientific trial, Nutrition 28:160�164, 2012. Braga M, et al: Enhanced recovery after surgery pathway in patients present process pancreaticoduodenectomy, World J Surg 38:2960�2966, 2014. Brennan M, et al: A prospective randomized trial of total parenteral diet after main pancreatic resection for malignancy, Ann Surg 220:436�444, 1994. Bruera E, et al: Cachexia and asthenia in cancer patients, Lancet Oncol 1:138�147, 2000. Bruix J, Sherman M; American Association for the Study of Liver Diseases: Management of hepatocellular carcinoma: an update, Hepatology 53(3):1020�1022, 2011. Bulger E, et al: Enteral vitamin E supplementation inhibits the cytokine response to endotoxin, Arch Surg 132:1337�1341, 1997. Bulger E, Helton W: Nutrient antioxidants in gastrointestinal illness, Gastroenterol Clin North Am 27:403�419, 1998. Burra P, et al: Hepatic malondialdehyde and glutathione in end stage chronic liver disease [abstract], Hepatology 16(4 Pt 2):266, 1992. Buzby G, et al: Prognostic nutritional index in gastrointestinal surgical procedure, Am J Surg 139:160�167, 1988. Cabr� E, et al: Effect of total enteral vitamin on the short-term end result of severely malnourished cirrhotics, Gastroenterology 98:715�720, 1990. Cerwenka H, et al: Normothermic liver ischemia and antioxidant therapy during hepatic resections, Free Radic Res 30:463�469, 1999. Cho M, et al: Vitamin D deficiency and prognostics among sufferers with pancreatic adenocarcinoma, J Transl Med eleven:206, 2013. Clugston A, et al: Nutritional danger index predicts a high-risk population in patients with obstructive jaundice, Clin Nutr 25(6):949�954, 2006. Cohendy R, et al: Preoperative dietary analysis of elderly patients: the Mini Nutritional Assessment as a practical tool, Clin Nutr 18(6):345�348, 1999. Curran R, et al: Multiple cytokines are required to induce hepatocyte nitric oxide manufacturing and inhibit protein synthesis, Ann Surg 212:460�471, 1990. Cywes R, et al: Effect of intraportal glucose infusion on hepatic glycogen content and degradation and consequence of liver transplantation, Ann Surg 216:235�247, 1992.
Purchase glyset with american express
This is due partly to a trend towards surgical specialization and centralization of care at high-volume establishments, the place the inverse volume-outcomes relationship has been nicely described for lots of advanced procedures (Finks et al, 2011; Nathan et al, 2009; Stitzenberg et al, 2009; Valero et al, 2015). Despite the observed lower in postoperative mortality, morbidity has remained primarily unchanged, with most giant collection reporting a 35% to 45% main complication price following both pancreatic or hepatic resection (Cameron & He, 2015; Kneuertz et al, 2012; Nathan et al, 2009; Vin et al, 2008). This widening gap between morbidity and mortality implies an improved capability to manage postoperative issues when they happen, thereby rescuing sufferers who previously would have died (Bassi et al, 2001; Sohn, 2003). This is partially due to earlier and more effective detection based mostly on familiarity with procedure-specific complications and advances in high-quality imaging. Another reason is the shift in administration from operative reexploration to interventional and endoscopic strategies which are efficient with much less added morbidity (Sohn, 2003; Vin et al, 2008). Interventional radiologists now make up an indispensible part of the multidisciplinary team caring for sufferers present process complicated hepatopancreatobiliary procedures and their experience within the minimally invasive treatment of anastomotic leaks, intraabdominal abscesses, and postoperative bleeding is responsible for significantly improved affected person outcomes (Mezhir, 2013; Sohn, 2003). This article will present an overview of probably the most commonly reported postoperative problems associated with major pancreatic and hepatic resections, including a evaluate of the current definitions and grading systems used for reporting. It will then provide an in depth dialogue of the suitable management of each complication in accordance with essentially the most current literature and with an emphasis on interventional strategies. The reported morbidity and mortality following pancreatic resection in a quantity of giant sequence reported since 2000 is offered in Table 27. Pancreatic resection is related to a bunch of issues, a lot of that are process specific and occur at the operative web site (hemorrhage, leak, obstruction), whereas others happen remotely as a consequence of main surgical procedure somewhat than the specific kind of surgery (deep venous thrombosis, cardiac arrhythmia, pneumonia). This article is primarily involved with the commonest extreme issues instantly related to the technical elements of the operation itself. The reported frequencies of those problems are listed in the reported frequencies for these complications in several massive series since 2000 are introduced in Table 27. Defining and Grading Complications After Pancreatectomy Postoperative issues are notoriously troublesome to examine because of the inconsistent definitions and imprecise terminology used to designate them (see Chapter 66). They comprise three overlapping manifestations of the identical underlying issue, which is breakdown and leakage on the pancreatic anastomosis (or pancreatic closure website for distal and central pancreatectomies). For example, an intraabdominal fluid assortment requiring drain placement might reasonably be reported as an abscess. If the drainage was studied and found to be amylase rich, it could probably be thought of a leak. If drainage from the leak continued throughout a time period, it could additionally be considered a fistula. However, the absence of any standardized, quantifiable measures for reliably differentiating these from one another meant that the identical complication might be reported in three different ways. They generated four consensus definitions consultant of those most commonly used within the literature and applied every to the same control group of pancreatectomies. Using these four definitions, the incidence of pancreatic fistulae various within the identical group of patients from 10% to 29%. This lack of consistency is mirrored in the literature, the place the actual reported incidence of pancreatic fistulae varies similarly from 2% to 29% (Braga et al, 2011; B�chler et al, 2000; Muscari et al, 2006; Reid-Lombardo et al, 2007). Regardless of the problem inherent in defining complications, accurate measurement and documentation in a standardized method is significant to improving high quality of care by permitting meaningful comparisons between procedures, institutions, and even particular person surgeons. This approach provides a simplified, unifying definition for each complication, with grades of increasing severity based upon the clinical influence of the complication and the invasive of the required therapy. Note that the grade of the complication will increase solely when a model new, more invasiveness or aggressive treatment is required for management. An example of this within the surgical literature is the development of the Clavien-Dindo classification of surgical complications. Clavien and colleagues (1992) acknowledged the inconsistency in reporting surgical issues in 1992 and proposed a definition and classification system for grading them in a standardized fashion. A complication, as outlined by Clavien, is any deviation from the normal postoperative course and is differentiated from a sequela, which is an "after-effect" of surgical procedure inherent to the process. The system was up to date in 2004 because the ClavienDindo classification, which is a graded system of increasing severity decided by the presumed long-term penalties of a given complication as properly as the invasiveness, degree of care, and sources required for the intervention needed to right it (Dindo et al, 2004). The system is made up of five grades, two of which have subgroups, and a suffix "d" class that can be appended to any grade.

Generic 50mg glyset otc
If the biliary stricture could be crossed, an internal/external biliary drain is placed, which has side holes each above and beneath the obstruction. Biliary drains are sometimes exchanged each 3 months to prevent clogging however are exchanged more frequently if cholangioplasty or different interventions are planned. If the bile duct damage has resolved on the cholangiogram, then an external biliary drain could be positioned to maintain access to the bile ducts. If the patient passes the capping trial (no fever, no significant leakage around the tube, no rise in bilirubin), then the drain could be safely eliminated. Nonsurgical management of benign biliary strictures are usually managed with endoscopic placement of a plastic biliary stent, or percutaneous internal/external biliary drainage. Cholangioplasty can be carried out using a high-pressure balloon throughout biliary drain placement or trade. High pressures and prolonged cholangioplasty (as long as 15 minutes) are sometimes required to overcome the dense fibrous tissue round biliary strictures. An 8-mm balloon can be used for intrahepatic strictures and a 10- to 12-mm balloon for widespread duct strictures. Cholangioplasty could be repeated at 2- to 14-day intervals (Cantwell et al, 2008; Zajko et al, 1995). For benign biliary strictures, cholangioplasty and internal/external biliary drainage have a long-term (25 years) main success rate of 59% and a secondary success fee of 80% (Cantwell et al, 2008). Failure of these approaches in in any other case healthy sufferers ought to prompt consideration of operative administration (see Chapter 42). Malignant biliary obstruction can be relieved with a biliary drainage catheter, to treat cholangitis, pruritus, or to decrease bilirubin for chemotherapy. A metal biliary stent may be positioned (percutaneously or endoscopically) for palliation of unresectable symptomatic biliary obstruction in patients with restricted life expectancy. Metal biliary stents positioned for malignant obstruction stay patent for a median of 11 months (Dahlstrand et al, 2009). Bleeding Complications See "Angiography, Embolization, and Covered Stent Placement," earlier. Chapter 27 Postoperative complications requiring intervention: analysis and administration 474. Adham M, et al: Central pancreatectomy: single-center expertise of fifty cases, Arch Surg 143:175�180, dialogue 180�181, 2008. Arita J, et al: Randomized clinical trial of the impact of a saline-linked radiofrequency coagulator on blood loss during hepatic resection, Br J Surg 92(8):954�959, 2005. Bassi C, et al: Management of issues after pancreaticoduodenectomy in a high quantity centre: outcomes on 150 consecutive sufferers, Dig Surg 18(6):453�457, discussion 458, 2001. Braga M, et al: A prognostic score to predict main issues after pancreaticoduodenectomy, Ann Surg 254(5):702�707, dialogue 707�708, 2011. B�chler M, et al: Role of octreotide in the prevention of postoperative issues following pancreatic resection, Am J Surg 163(1):125� a hundred thirty, discussion 130�131, 1992. Cope C, et al: Percutaneous management of continual pancreatic duct strictures and exterior fistulas with long-term outcomes, J Vasc Interv Radiol 12(1):104�110, 2001. Correa-Gallego C, et al: Contemporary experience with postpancreatectomy hemorrhage: outcomes of 1,122 patients resected between 2006 and 2011, J Am Coll Surg 215(5):616�621, 2012. Cozzi G, et al: Percutaneous transhepatic biliary drainage in the administration of postsurgical biliary leaks in sufferers with nondilated intrahepatic bile ducts, Cardiovasc Interv Radiol 29(3):380�388, 2006. Crippa S, et al: Middle pancreatectomy: indications, short- and longterm operative outcomes, Ann Surg 246:69�76, 2007. Darwin P, et al: Jackson Pratt drain fluid-to-serum bilirubin focus ratio for the diagnosis of bile leaks, Gastrointest Endosc 71(1):99� 104, 2010. Dindo D, et al: Classification of surgical complications: a model new proposal with analysis in a cohort of 6336 sufferers and outcomes of a survey, Ann Surg 240(2):205�213, 2004. Epelboym I, et al: Quality of life in sufferers after complete pancreatectomy is comparable with high quality of life in patients who undergo a partial pancreatic resection, J Surg Res 187:189�196, 2014. Erdogan D, et al: Incidence and management of bile leakage after partial liver resection, Dig Surg 25(1):60�66, 2008. Ernst O, et al: Biliary leaks: therapy by means of percutaneous transhepatic biliary drainage, Radiol 211(2):345�348, 1999. Friess H, et al: Randomized managed multicentre study of the prevention of issues by octreotide in sufferers undergoing surgical procedure for chronic pancreatitis, Br J Surg 82(9):1270�1273, 1995. Gr�tzmann R, et al: Evaluation of the International Study Group of Pancreatic Surgery definition of post-pancreatectomy hemorrhage in a high-volume center, Surgery 151(4):612�620, 2012.
Order 50 mg glyset with amex
Surgeons should indicate in operative notes for open and laparoscopic cholecystectomy precisely how they recognized the cystic buildings for division. For conversions, they need to specify the circumstances, stressing safety and surgical judgment. When prospectively adopted, data suggest that more than one third of asymptomatic stones will cross spontaneously after the primary 6 weeks after cholecystectomy (Collins et al, 2004). These are very delicate (96% to 98%) but not very particular (0% to 70%) (Koo & Traverso, 1996). The technical success fee of percutaneous radiologically guided cholecystostomy is 98% to one hundred pc with few procedure-related complications (mortality and main issues, 0% to 6. Potential issues include intrahepatic hematoma, pericholecystic abscess, and biliary peritonitis and pleural effusion attributable to puncture of the liver and subsequent migration of the catheter (Yamashita et al, 2013). Timing of Subsequent Operation for Cholecystitis Once the inflammatory course of has resolved, elective cholecystectomy could be carried out early (within 1 to 7 days) or delayed (6 to 8 weeks) with glorious success and conversion charges as little as 3% (Akyurek N, 2005). Some have reported utilizing percutaneous cholecystostomy as definitive therapy for acute cholecystitis in highrisk, elderly, and debilitated sufferers. For sufferers present process cholecystectomy for symptomatic gallstones, the prevalence of choledocholithiasis ranges from 10% to 18% (Dasari et al, 2013). When overused, most cholangiograms are normal, and costs and complication charges are prohibitive. Surgeons can respond to such findings, flushing the duct to clear stones or particles. Other advised advantages specifically relate to the prevention of bile duct injuries (Fletcher et al, 1999). The randomized trials which were performed to tackle this query are small, and even a systematic evaluation of these trials was not sufficiently powered to show a significant benefit (Ford et al, 2012). In persistent situations, and relying on the extent and period of biliary obstruction, choledocholithiasis may also result in secondary biliary cirrhosis and portal hypertension. For sufferers who fail nonoperative treatments, surgical drainage may be needed (see Chapters 31 and 36A). Laparoscopic ultrasound cholangiography is also efficacious but not broadly used, and its utility is proscribed by its longer studying curve (Stiegmann et al, 1995). Newer techniques similar to hyperspectral cholangiography and near-infrared fluorescence cholangiography hold promise and should turn out to be extra broadly used in the future (Buddingh et al, 2011). Ultimately, the selection of modality depends on native availability and experience in minimally invasive remedies coupled with considerations of value and convenience. The most constant danger issue for failing transcystic stone clearance is the scale of the stone. Once stones exceed 5 mm, the chance of transcystic extraction falls considerably (Stromberg et al, 2008), and laparoscopic choledochotomy turns into essential. Gallstone Pancreatitis Acute gallstone pancreatitis is probably the most frequent form of acute pancreatitis in Western countries (see Chapters fifty four and 55). The two mostly accepted mechanisms for the pathogenesis of gallstone pancreatitis are reflux of bile into the pancreatic duct and transient ampullary obstruction attributable to short-term impaction of a stone within the ampulla. These patients should undergo elective cholecystectomy once the pancreatitis has resolved. At the opposite finish of the spectrum are sufferers with gallstone pancreatitis and associated acute cholangitis (see Chapter 43). Clear evidence reveals that endoscopic biliary drainage is useful in sufferers with acute cholangitis; thus these patients ought to have early biliary decompression. A secondary query is whether or not or not patients with gallstone pancreatitis, with out cholangitis, benefit from biliary decompression. Clinical and experimental studies suggest that impacted ampullary stones and persistent biliopancreatic obstruction are related to a extra extreme medical course. In theory, early endoscopic removal of obstructing ampullary gallstones should enhance outcomes (Acosta et al, 1997; Alexakis et al, 2007). The function of nonsurgical intervention, prior to definitive surgical therapy, has been examined in a number of prospective randomized studies during which patients with cholangitis were excluded. Integral to any interpretation of therapy method is the severity of the gallstone pancreatitis. The Ranson and Glasgow standards have the benefit of ease of use and considerable areas of overlap (Table 37.

Cheap 50mg glyset mastercard
In the identical report, a second affected person introduced with cholangitis and was reported to be cured following a left hepatectomy for papillomatosis confined to the left intrahepatic duct. A review of 78 circumstances by Yeung and colleagues (2003) confirmed a male to feminine ratio of approximately 2: 1, with a mean age at presentation of 63 years (range, 6 to eighty three years). Almost half the sufferers (42%) had diffuse intrahepatic and extrahepatic disease, and 27% had only intrahepatic illness; one other 27% had only extrahepatic disease, and two patients had involvement of the gallbladder. Only 55% of the patients have been candidates for a curative resection, and the rest have been palliated in various ways, together with choledochoscopic laser ablation, iridium-192 intraluminal therapy, percutaneous cholangioscopic electrocoagulation, and combined cholangioscopic laser ablation and external beam radiotherapy. Cattell and Pyrtek (1950) suggested that these lesions had a low-grade malignant potential after reporting recurrence of obstructive jaundice in a patient inside a 12 months of present process successful placement of a T-tube. Padfield and colleagues (1988) documented basement membrane discontinuities in three sufferers consistent with patterns accompanying malignant tumors; they cautioned that papillary neoplasms, although histologically benign, must be thought-about premalignant. The extent, distribution, and secondary obstructive changes induced by these lesions present therapeutic challenges. If the lesions are limited and confined to one facet of the liver, resection ought to be strongly thought of. Gouma and colleagues (1984) had been capable of trace 12 sufferers with adequate obtainable follow-up and located a imply survival of 28 months. However, though no affected person survived greater than 6 years, 5-year survival was seen only in three sufferers submitted to radical surgery. It seems clear that even main resectional surgical procedure for this lesion has a excessive recurrence fee. A 67-year-old woman with papillomatosis and high-grade dysplasia occluding the left hepatic duct was efficiently managed by a left hepatic lobectomy (Helling & Strobach, 1996). The authors reviewed the literature and commented on three essential features of this lesion: (1) a excessive recurrence price, with approximately 50% of patients requiring reoperation; (2) copious mucin manufacturing which will lead to fluid electrolyte imbalances; and (3) malignant transformation, which is noticed in a major proportion of patients. Using the strategy described by Hutson and colleagues (1984) and Barker and Winkler (1984) appears reasonable: a Roux-en-Y hepaticodochojejunostomy is common in such a way as to permit a jejunal fistula for entry to the biliary tree postoperatively and allow repeated curettage or intubation (see Chapters 31 and 42). Meng and associates (1997) reported on using holmium: yttriumaluminum-garnet laser therapy by way of choledochoscopy and profitable ablation after curettage; after four sessions, all tumor was ablated, with no signs of tumor recurrence at 6 months. Because of deteriorating liver perform, she underwent profitable orthotopic liver B. The last pathology revealed three foci of invasive carcinoma restricted to the biliary wall. After 22 months of follow-up, the patient remained asymptomatic, with out proof of tumor recurrence or metastasis. In abstract, an inexpensive strategy to the uncommon condition of a quantity of biliary papillomatosis contains preoperative and operative cholangiographic analysis, early choledochotomy, and assessment of the intrahepatic biliary tree by choledochoscopy. If the tumor is bulky, curettage is performed to identify the sites of origin within the bile duct. Care must be taken to carry out choledochoscopy of as many intrahepatic ducts as attainable. It seems best to avoid long-term exterior drainage as a preliminary palliative process, and curettage or inside bypass is indicated. Some form of hepaticojejunostomy could additionally be useful as a result of it allows percutaneous entry to the biliary tract. First desribed in 1926 as granular cell myoblastoma, latest debate has ensued in regards to the cell of origin. Levy and colleagues (2002) suggested that, somewhat than myoblasts, the tumor may originate fom Schwann cells, evidenced by its immunohistochemical staining with antibodies to S-100 protein normally discovered within the central nervous system or in Schwann cells in the peripheral nervous system. Honjo and colleagues (2003) reported a case of extrahepatic biliary schwannoma, basing this diagnosis on S-100 positivity on immunohistochemistry. More than 80% of documented circumstances have occurred in feminine patients, 66% of whom are black, and 15% of sufferers have multiple lesions (Vance & Hudson, 1969). Clinical symptoms associated with granular cell myoblastoma arising in extrahepatic bile ducts are most likely to be these of painless jaundice, and a presentation of higher belly ache and colic is extra regularly associated with lesions arising in the cystic duct. Granular cell myoblastoma could be included within the differential analysis of obstructive jaundice seen in a black feminine, especially if she has a tumor nodule in the tongue, breast, or subcutaneous tissue, but such a clinical presentation could be extraordinarily uncommon. On minimize section, granular cell myoblastoma is yellowish white, and microscopically it consists of fibrous tissue diffusely infiltrated by giant, elongated polygonal cells or cells containing small, darkish nuclei and an abundant eosinophilic granular cytoplasm on hematoxylin and eosin stain. The tumor was initially termed granular cell myoblastoma because it was thought to be derived from "myoid cells.
Discount 50 mg glyset with amex
A 5 mm digicam can then be inserted at this web site to better consider any adhesions which may be present alongside the midline. If essential, right upper quadrant or subxiphoid ports could additionally be inserted subsequent to free adhesions from the midline earlier than a trocar and digicam are inserted in that place. Cirrhosis Cirrhosis is taken into account by many to be a contraindication to at least laparoscopic cholecystectomy, and probably to cholecystectomy normally (see Chapter 77). This is as a outcome of of considerations over the flexibility to retract a heavy, friable liver, and the chance of coagulopathy. A recent population-based examine demonstrated that the laparoscopic approach is nicely tolerated by sufferers with cirrhosis and related to considerably decrease rates of infection, bleeding, transfusion, liver failure, and total mortality compared with an open procedure, making it the procedure of selection for cholecystectomy (Chmielecki et al, 2012). To successfully carry out a cholecystectomy in a patient with cirrhosis, any coagulopathy should be reversed earlier than surgical procedure. Careful attention should be made to observe for any aberrant portosystemic venous collateralization, both in the liver bed, porta hepatis, and even in the abdominal wall. Liberal use of hemostatic brokers can be utilized, and power sources, including the argon beam cautery ought to be available if needed. Once the process is full, consideration must be placed to rigorously ensure that all incision closures are made watertight to decrease postoperative ascitic leak (Poggio et al, 2000). A surgeon whose primary experience is with open cholecystectomy may more liberally convert, whereas many younger surgeons at present have solely a restricted expertise with the open approach and feel more comfortable utilizing advanced laparoscopic strategies to troubleshoot problems or accomplish the procedure. Although conversion rates are generally larger with less skilled surgeons, a nationwide study reported a conversion fee to open procedure of 5% to 10% (Livingston & Rege, 2004). Primary reasons to contemplate a conversion embrace unclear anatomy, intraoperative complications, failure to progress in a timely method, and pathology, together with choledocholithiasis not amenable to laparoscopic or postoperative endoscopic techniques (see Chapters 36 and 37). Although conversion has been thought of a "complication" by some, it ought to be regarded as mature judgement, accepting a probably longer hospital stay to keep away from a disastrous complication. Often the problems requiring conversion to open laparotomy are obvious, including large hemorrhage, bowel perforation, or main harm to the bile duct. An open process provides the advantage of palpation and tactile sensation to the surgeon. This could additionally be useful when the anatomy is unclear from inflammation, adhesions, or anomalies. Although rare, the invention of a fistula between the biliary system and bowel may require laparotomy for definitive administration. This incision is made 2 cm beneath the costal margin and customarily extends from the midline to the edge of the rectus muscle laterally. The length of the incision must be tailor-made to the publicity required and physique habitus of the affected person. The rectus muscle is divided with cautery, ensuring appropriate hemostasis by any perforating vessels in the muscle. The posterior rectus sheath is incised, and the stomach is entered Exposure and Placement of Retractors Exposure during open cholecystectomy is paramount to performing the procedure adequately and safely. The round ligament is divided between ties or, sometimes, with an energy-sealing system close to the anterior stomach wall. The falciform ligament is incised with cautery for several centimeters superiorly to additional facilitate exposure. A main retractor similar to a Thompson- or Bookwaltertype retractor is then hooked up to the working room table and correctly arrange. Two abdominal wall retractors are positioned on the superior fringe of the incision, one medially and one laterally, and secured to the retractor system. Moist sponges are used to pack the bowel out of the operative field inferiorly, and additional packs positioned behind the liver usually help elevated the gallbladder into the sector for easier dissection. Gallstones and Gallbladder Chapter 35 Technique of cholecystectomy: open and minimally invasive 577 always needed in a small affected person. An extra retractor is then positioned on the undersurface of the liver to the left of the gallbladder to retract the liver edge out of the finest way and bring the porta hepatis into view. Dissection Retrograde Cholecystectomy When performing a retrograde cholecystectomy, the crucial view of security is first recognized earlier than removing of the gallbladder from the liver. This approach is the identical old technique used throughout laparoscopic cholecystectomy however may be more challenging for a novice surgeon within the open setting without the magnification of laparoscopy and when exposure is difficult secondary to irritation or weight problems. However, it is important to preserve the same principles to keep away from inadvertent biliary injury. The incision is carried alongside anteriorly and posteriorly to exposure the cystic triangle.
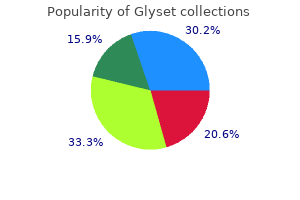
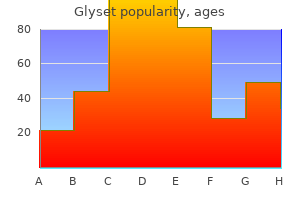
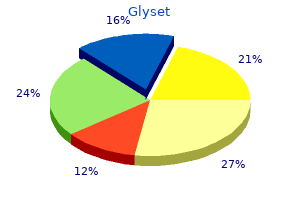
Real Experiences: Customer Reviews on Glyset
Harek, 46 years: Although these tumors sometimes come up within the adrenal gland as pheochromocytoma, extraadrenal lesions are extra frequently discovered in the neck, within the mediastinum, and at the aorta close to the origin of the inferior mesenteric artery.
Avogadro, 55 years: They go away as freeswimming cercariae that subsequently connect to watercress, water lettuce, alfalfa, mint, parsley, or khat.
Merdarion, 29 years: Additionally, sufferers pretreated with sincalide earlier than cholescintigraphy paradoxically appear to be extra more doubtless to reveal a nonpathologic delay in biliary transit into bowel, at least if sincalide is infused comparatively rapidly (Kim et al, 1990).
Garik, 60 years: Crosstalk between the innate and adaptive immune techniques bridges the nonspecific initial response to a highly specialized system able to long-lasting immunologic reminiscence.
Vigo, 22 years: Todani T, et al: Hepaticoduodenostomy at the hepatic hilum after excision of choledochal cyst, Am J Surg 142:584�587, 1981.
Campa, 62 years: Sometimes adjacent enhancing liver parenchyma compressed by a cyst might mimic the appearance of an enhancing wall, inflicting diagnostic ambiguity.
9 of 10 - Review by Y. Cole
Votes: 49 votes
Total customer reviews: 49
References
- Nawrot TS, Perez L, Kunzli N, et al. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet 2011; 377: 732-740.
- Papaemmanuil E, Gerstung M, Malcovati L, et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood. 2013;122:3616-3627; quiz 99.
- Rizvi NA, Hellmann MD, Snyder A, et al. Cancer immunology. Mutational landscape determines sensitivity to PD- 1 blockade in non-small-cell lung cancer. Science 2015;348(6230):124-128.
- Sperduto PW, Wang M, Robins HI, et al. A phase 3 trial of whole brain radiation therapy and stereotactic radiosurgery alone versus WBRT and SRS with temozolomide or erlotinib for non-small cell lung cancer and 1 to 3 brain metastases: Radiation Therapy Oncology Group 0320.

