Isoniazid dosages: 300 mg
Isoniazid packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Isoniazid 300 mg mastercard
A, Lateral radiograph of mandible with lytic lesion produced by expanding nerve sheath tumor arising in affiliation with mandibular nerve. B, Radiograph of expansile tumor of pubic ramus in younger adult with lengthy history of groin ache. Inset, Sagittal computed tomogram exhibiting thinning of superior orbital bone by schwannoma (arrow). A, Low power photomicrograph displaying densely cellular (Antoni type A) and hypocellular (Antoni kind B) components of schwannoma (�100). C, Intermediate power photomicrograph showing nuclear palisades (Verocay bodies) in schwannoma (�200). D, Expression of S-100 protein in schwannoma (Verocay bodies) revealed by immunohistochemistry (�200). A, Spindle cells with plentiful cytoplasmic processes surrounded by basal lamina (�4000). B, Higher magnification of interdigitating cytoplasmic processes with basal lamina. Mutations within the region that directly affect the R1276 residue and change the conformational standing of the area activate the Ras pathway just like oncogenic mutations instantly affecting the Ras protein. This creates a hypersensitive environment with aberrant morphogenesis of nerves and hyperproliferation of both fibroblasts and endothelial cells. Clinical Symptoms Clinical presentation of neurofibromatosis kind 1 is very variable, but a mixture of cardinal signs, listed in Table 14-3, should be current to establish the prognosis of this syndrome. Typically, the illness turns into evident in the course of the first few years of life and is recognized by the presence of dermatologic or ophthalmic lesions when caf� au lait spots and Lisch nodules develop. Initially, the pores and skin lesions resemble freckles, however they enlarge with age and turn into darker, predominantly involving the areas unexposed to sun. The presence of multiple skin neurofibromas is the hallmark of fibromatosis kind 1 and so they sometimes develop throughout childhood after the caf� au lait spots turn into evident. Some of these tumors are evident at start; others continue to develop through late maturity. They contain each superficial and deep nerves, and the signs may be related to the involvement of nerves in various organs and anatomic websites. The affiliation of neurofibromatosis sort 1 with schwannoma, pheochromocytoma, ganglioneuroma, nephroblastoma, gastrointestinal stromal tumor, and leukemia has been reported. Variants of neurofibromatosis kind 1 with incomplete or aberrant features in medical presentation embody segmental manifestation, manifestation restricted to gastrointestinal or spinal involvement, and the so-called "familial" caf� au lait spots. Eventually, greater than 30% of sufferers with neurofibromatosis type 1 develop these lesions. The number and size of caf� au lait spots correspond to some extent to the severity of the disease. Patients with much less prominent pores and skin pigmentation could have a later or much less severe onset of neurofibromatosis. The borders of the pigmented areas are much less irregular than those related to Albright-McCune syndrome ("coast of California" rather than "coast of Maine" contours). Microscopically, caf� au lait spots are characterised by an elevated stage of pigmentation in the basal and peribasal layers of dermis. The presence of large melanosomes (macromelanosomes) is recommended by some authors to be pathognomonic for neurofibromatosis. Multiple localized neurofibromas that form discrete nodules in the gentle tissue are the commonest lesions in well-developed circumstances of neurofibromatosis type 1. Nodular localized neurofibromas in neurofibromatosis are often bigger than solitary neurofibromas unassociated with neurofibromatosis. A, Facial cutaneous and subcutaneous neurofibromas in young man with comparatively few skin lesions. B, Caf� au lait skin pigmentation in discrete, nonconfluent distribution over trunk.
Buy 300 mg isoniazid visa
Morpheaform basal cell carcinomas produce stiffness, thickening, and scaliness of the skin, thus mimicking scleroderma. Although most of these sufferers truly have solely actinic shrinkage, morpheaform basal cell carcinoma can also produce skin contracture. Many patients have been handled for easy cicatricial ectropion once they actually have invasive morpheaform basal cell carcinoma, which can trigger the pores and skin to turn into indurated and thickened. When repairing any cicatricial ectropion that involves sun-damaged skin, tissue ought to be submitted for histologic examination. B, Another patient was initially recognized with ectropion but was later found to have morpheaform basal cell carcinoma. More extensive distortion of the lashes across the lid margin might seem as upper lid entropion. Purely dermatologic conditions such as rosacea can yield comparable outcomes, but neoplastic disease could have to be ruled out in some sufferers whose circumstances demonstrate a refractory scientific course. The most insidious neoplasm that presents in this manner is sebaceous cell carcinoma, which additionally typically entails pagetoid changes. Another neoplastic course of that happens within the periocular space, that has neurotropic tendencies, and that will lengthen to the eyelids is carcinoma of the lacrimal gland. The biopsy confirmed infiltrative squamous cell carcinoma with perineural invasion of the infraorbital nerve. B, the biopsy of the best supraorbital nerve (arrows) confirmed perineural invasion. The patient died of cardiac arrest, and no postmortem permission for post-mortem could probably be obtained. The danger of missing an underlying neoplasm is at all times attainable if a superficial biopsy is taken of a suspicious eyelid lesion. If the tumor is comparatively small, excisional biopsy of the entire lesion could additionally be performed. In many instances, a wedge of a larger tumor may be excised as a biopsy specimen as a preliminary step for Mohs surgical procedure. B, A full-thickness biopsy of the eyelid margin have to be obtained to detect any intralid processes. Special staining strategies may help to differentiate intraepithelial lesions, corresponding to sebaceous cell carcinomas, squamous cell carcinomas, and superficial basal cell carcinomas. Epithelial biopsies are often misinterpreted with regard to the exact kind of tumor. For example, squamous cell carcinoma may be identified when the lesion is a sebaceous gland carcinoma with pagetoid skin changes. Such microscopic evaluation could also be performed by examining frozen sections at the time of surgery, which permits the surgeon to immediately take away additional tissue if the tumor is histologically current at the margin of the incision. In the case of tumors similar to basal cell carcinomas, which usually grow from a single focus, a really high remedy price may be achieved if the extent of resection is managed by frozen part examination of the margins. For patients in whom the histologic margin of the tumor extends into the orbit, orbital exenteration or irradiation may be required. With malignant eyelid tumors that are multicentric in origin, corresponding to sebaceous cell carcinomas, it is in all probability not attainable to utterly rely on the examination of resection margins, as a outcome of only one focus of the lesion may be removed. For tumors that cause early distant metastases, such as nodular melanomas, clear margins supply no guarantee against regional or systemic metastatic disease. The two techniques carried out in these areas differ with regard to the strategies of sectioning and examining the margins, which are described in the following sections. We resect the primary tumor with gross margins free of tumor, relying on the tumor sort. We then ship additional margins for frozen part analysis, with instant reexcision occurring if the results are positive. The dermatologic surgeon performs the excision and sectioning with tumor mapping till clearance is obtained. This allows the pathologist to set up the characteristics of the specific lesion.
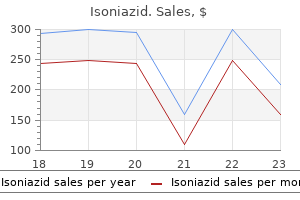
Order isoniazid 300 mg with amex
Skin dissection and undermining is carried out until the lid may be repositioned to its normal position. The pores and skin graft is positioned within the recipient area and then fixated to the periosteum either laterally or nasally, on the medial canthal tendon. A and B, the subciliary incision for a grafted medial canthus should prolong past the canthus. E and F, the horizontal tightening procedure is commonly combined with pores and skin grafting. B, the affected person is shown after fixation of a full-thickness sling graft to the lower lid. Chapter 30 � Cicatricial Ectropion and Entropion 883 Technique A extensive subciliary incision that extends past the canthal areas is made that will expose the canthal tendon medially and the orbital rim periosteum laterally. In many circumstances, nevertheless, these flaps should be supplemented with a free skin graft within the central area. Technique Horizontal transposition flaps, wanted for lid stabilization and based mostly on the canthus within the higher lid, are outlined after subciliary incisions have been made within the decrease lid. C and D, Transposition and suturing of the flaps on the medial and lateral canthi. For patients with extra distinguished eyes, tightening or stiffening of the lower lid by the previously described methods can produce a clotheslining effect on the lid. For these sufferers, a spacer graft combined with lateral horizontal tightening can be utilized within the posterior eyelid lamella to forestall clotheslining and to keep away from an externally visible skin graft. An incision is made beneath the inferior tarsus via the conjunctiva and inferior retractors, which are separated to produce the desired lid elevation. A spacer (ear cartilage or other) is then sutured into the created defect, which produces elevation of the decrease lid to the desired level. This technique, when combined with supraplacement of the lateral canthal tendon, ought to appropriate lower lid retraction in a prominent eye. These complicated instances of ectropion are generally seen after surgical procedures for orbital eyelid trauma. Contracture of the orbital septum and capsulopalpebral fascia is often an important issue in the pathogenesis of complicated cicatricial ectropion. In most of those instances, malposition of the decrease lid can be corrected only with grafting of each the external and inside eyelid lamella. If sufficient muscle tissue is current, it can be interposed between the grafts to present an adequate blood provide. Chapter 30 � Cicatricial Ectropion and Entropion 887 Technique A posterior incision is made on the inferior tarsal edge, and the adhesions are dissected with upward retraction. The inferior incision must be under the inferior marginal artery, leaving the nasal blood provide intact to make sure the survival of the margin. Next, an incision is made across the subciliary area, with dissection of the pores and skin or skin-muscle flap away from the lid. B, Correction of a bilevel contracture with a bilevel inside spacer and skin grafting (or vertical recruitment of external skin). B, the patient after multiple procedures of bilevel grafting with spacer insertion. Technique A full-thickness blepharotomy is made on the bottom fringe of the phase needed for rotation. He is a candidate for pores and skin alternative of the external lamella in a traditional ectropion repair. The patient is a candidate for pores and skin substitute of the external lamella in a standard ectropion repair, however he can also need resection of the damaged eyelid margin. This patient may profit from lower lid reconstruction procedures, in addition to pores and skin grafting. However, a histologic control excision of the basal cell carcinoma with eyelid reconstruction procedures is indicated.
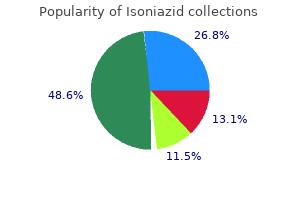
Isoniazid 300mg low price
The results of those procedures are unpredictable, and it might take as long as 3 to 4 years to produce any discernable results. However, it has a lot much less of an effect on the eyelids and causes a practical deficit in the utilization of the tongue with hemiglossal atrophy. Splitting the hypoglossal nerve by not more than 40% minimizes the quantity of ensuing motor deficit to the tongue while providing sufficient reinnervation to the facial nerve. For sufferers with prolonged denervation time (greater than 6 months), a partial hypoglossal to facial nerve anastomosis can "babysit" the facial nerve to prevent atrophy and lack of motor endplates whereas axonal progress from cross-facial nerve grafting is completed. Use of the masseter nerve also avoids practical deficits and atrophy of the tongue. Compensatory eyeLid sUrgery Reinnervation procedures give hope for the future within the rehabilitation of patients with facial paralysis. As a practical matter, nevertheless, the eyelids appear notably unresponsive, and most sufferers ultimately bear eyelid procedures to help improve eyelid closure or position. Compensatory eyelid surgical procedure entails three areas: the lower lid, upper lid, and eyebrow. Facial nerve palsy with eyelid involvement can happen from many causes and may be short-term or everlasting. Regardless of the cause, the primary precedence is safety of the eye, and each temporizing and permanent procedures are available to accomplish this. In long-standing circumstances, these procedures may also restore some normalcy to facial appearance. Close follow-up will determine the diploma of return of perform, which is usually very favorable. Effectiveness of the gold weight trial process in predicting the perfect weight for lid loading in facial palsy: a prospective examine. Quantitative measurement of evolution of postparetic ocular synkinesis treated with botulinum toxin kind A. Three-dimensional video evaluation of the paralyzed face reanimated by cross-face nerve grafting and free gracilis muscle transplantation: quantification of the practical consequence. Outcomes of periocular reconstruction for facial nerve paralysis in most cancers patients. M�llerectomy for upper eyelid retraction and lagophthalmos because of facial nerve palsy. External lid loading for the momentary treatment of paresis of the M orbicularis oculi: a case report. Treatment of symptomatic facial nerve paralysis with lower eyelid fascia lata suspension. Electroneurography and intraoperative facial monitoring in contemporary neurotology. Modified approach for rehabilitation of facial paralysis using autogenous fascia lata grafts. Transient facial nerve palsy following bilateral sagittal break up ramus osteotomy for setback of the mandible: a review of incidence and administration. Long-term outcomes for the use of gold eyelid load weights in the management of facial paralysis. Reply: Upper eyelid postseptal weight placement for therapy of paralytic lagophthalmos. Upper eyelid postseptal weight placement for remedy of paralytic lagophthalmos. Restoration of the blinking reflex in facial palsy by a easy lid load operation. The outcomes of dynamic procedures for blink restoration in pediatric facial paralysis. Experience with the gold weight and palpebral spring in the administration of paralytic lagophthalmos. Minitendon graft switch for suspension of the paralyzed decrease eyelid: our expertise. Surgery must be averted within the active inflammatory section to keep away from potential further changes after surgery; if other rehabilitative procedures are needed, eyelid surgery should be performed in correct sequence with these procedures. This situation commonly causes contracture and stiffness of the eyelids, producing retraction that may end up in corneal exposure.
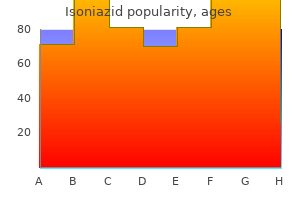
Buy isoniazid 300mg line
Plicated folds with cryptlike invaginations happen, and the stroma consists of fibrovascular connective tissue with lymphatic channels, capillaries, and formation of an episcleral venous plexus. The bulbar endothelial cell junctions turn out to be incompetent, thereby permitting extravascular extravasation of edema beneath the conjunctiva. The stimulus that initiates chemosis of the conjunctiva after blepharoplasty is more than likely caused by irritation and dryness ensuing from the surgical dissection and postoperative lagophthalmos, combined with a person predisposition to conjunctival edema. The explanation for chemosis is multifactorial, thereby making a cycle that begins with surgical procedure, adopted by impaired eyelid closure that results in exposure, resulting in desiccation and irritation of the conjunctiva. This, combined with lymphatic dysfunction and periorbital postoperative edema, results in chemosis. Depending on the degree of chemosis, extreme prolapse causes chemosis-induced lagophthalmos, which completes the circle back to increased exposure of the conjunctiva. This vicious cycle requires conservative intervention with ophthalmic antibiotic ointments to rehydrate the cornea and conjunctiva. The swelling additionally causes anatomic distortion at the interface between the eyelid and cornea, which can delay chemosis if not corrected. If lid malposition similar to ectropion is related to postoperative chemosis, a lateral canthoplasty is mostly required to close the house between the eyelid and lower lid. If the swollen conjunctiva seems to be inflicting the lower lid malposition, significantly on the corneoscleral limbus, tear flow shall be unable to reach the cornea. If the cornea turns into dry, thinning of the cornea will end in lack of surface epithelium and cause a dellen formation, which may be seen on slit-lamp examination with fluorescein uptake. Ophthalmic antibiotic ointment, patching, and drainage of the chemosis might be required to appropriate the mechanics. Dryness and publicity result in desiccation of nonkeratinized mucosal epithelium on the floor of the conjunctiva. A cyclic relationship of chemosis inflicting conjunctival prolapse and chemosis-induced lagophthalmos requires intervention for remedy. Chemosis associated with lid malposition or continual chemosis resulting from irregular eyelid closure biomechanics requires surgical correction of eyelid position and function before the chemosis can be resolved. There continues to be a need to define the structural injury that may happen to lymphatic channels draining the conjunctiva Chapter 17 � Management of Chemosis 471 throughout blepharoplasty from a skin-muscle flap and lateral canthal dissection. Therefore chemosis is found after transcutaneous lower blepharoplasty in addition to transconjunctival lower blepharoplasty. The incidence of chemosis is the same, whether or not a canthopexy or canthoplasty is carried out. If the chemosis seems to be mild and additional surgical procedure corresponding to a face carry is planned, ophthalmic ointment could be liberally utilized during surgical procedure; then a moistened eye pad may be taped to the closed eyes utilizing a Steri-Strip from the forehead to the cheek. Patients will be succesful of open their eyelids sufficient to see in the course of the first 7 days after surgical procedure. The interim marginal momentary tarsorrhaphy suture is eliminated on postoperative day 7, along with other blepharoplasty sutures that require elimination. For extra severe circumstances of chemosis which might be recognized at the time of surgery, 6-0 plain catgut suture can be utilized within the fornix to plicate the loose conjunctiva and stop outward herniation. D, A one-snip conjunctivotomy is performed, with drainage of the chemosis fluid either intraoperatively or postoperatively. Continued use of ophthalmic ointment and patching the attention closed at night time, with Steri-Strips utilized to help assist the lower eyelid, will shorten the restoration interval. This conservative technique corrects chemosis by restabilizing the conjunctival vasculature and decreasing inflammation. In some delicate circumstances, the chemosis could be immediately corrected in the course of the workplace go to. Patients are instructed to continue to use the eyedrops, mixed with patching the eyelids for 24 hours if possible; otherwise, at night. The eyepatch have to be accomplished correctly to completely shut the eyelids with out irritating the cornea with the patch.
ADT (Androstenetrione). Isoniazid.
- Improving athletic performance and other conditions.
- What is Androstenetrione?
- Are there safety concerns?
- Dosing considerations for Androstenetrione.
- How does Androstenetrione work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97037
Buy isoniazid now
G, An assistant can retract the pores and skin edges with cotton-tip applicators, and hemostasis is obtained with bipolar or unipolar electrocautery on a low setting. H, the orbital septum may be opened for its entire width with the scissors to visualize the preaponeurotic fats. J, the skin-muscle flap is excised with straight Iris scissors, beveling away from the crease and consistent with the previous skin incision. Conservative fat resection is important, especially the interpad fat between the central preaponeurotic fats and the nasal fats pad. The general quantity to take away is the fat that protrudes anterior to the orbital rim, with no counterpressure, when the patient is within the supine operative place. When the patient is standing postoperatively, this fats tends to protrude barely extra and forestall the formation of a hole sulcus. With anterior traction on the fats and downward traction on the lid, the preaponeurotic fat is dissected off the levator. If the patient is to have a concomitant ptosis repair, this publicity is essential. C and D, Downward traction on the lid helps to visualize the levator aponeurosis and the musculoaponeurotic junction. Adequate publicity for elimination of the nasal fats pad requires nasal retraction with Blair retractors and gentle strain on the corneal protector. A small nick in the bulging septum simply lateral to the artery causes herniation of the whitish coloured nasal fat pad. Once this happens, the nasal fat pad can be safely eliminated in a fashion much like removal of the aponeurotic fat, by dissecting the fat flush with the level of the orbital rim. This prevents a sunken nasal compartment postoperatively and helps to forestall entering the nasal orbit. F, With strain on the globe, the nasal fats pocket will prolapse and could be excised. H, Fat is excised with an electrocautery tip under direct visualization somewhat than with clamping and chopping. Chapter 7 � Upper Lid Blepharoplasty 245 We suppose that the normal technique of clamping, chopping, cauterizing the fat within the clamp, and releasing the fats into the orbit ought to be abandoned. B, Postoperatively, the higher lid crease ought to have a parallel, concentric curvature. The goal is to produce a steady lateral upper lid crease with out making the scar too lengthy and without leaving too much lateral tissue, which creates a fold lateral to the canthus. The lateral eyelid space lends itself to maximal skin excision, which is usually outlined by an ellipse that begins 6 to 7 mm above the lateral canthus and 10 to 15 mm under the nonplucked brow hairs on the junction of thick brow pores and skin and thin eyelid skin. Additional procedures may be necessary within the lateral forehead area to create a satisfying crease and contour without folds and fullness. In these instances, lacrimal gland ptosis may be corrected by retracting the lid and lateral horn of the levator downward and inserting plicating 6-0 Vicryl sutures from the lateral horn of the levator to the arcus marginalis anterior to the lacrimal gland. Downward retraction prevents the chance of suturing the lid open and creating iatrogenic lagophthalmos. Support of the lateral portion, or tail, of the forehead is usually necessary and missed. Mechanically, the brow acts like a curtain rod to the eyelid pores and skin; subsequently forehead stability is necessary to prevent downward migration leading to skin redundancy and residual folds. In different instances it extends farther down onto the lid into the preseptal space to contribute to higher lid fullness. Chapter 7 � Upper Lid Blepharoplasty 247 Abundant lateral brow fats can be sculpted away from the orbital rim. The fats is dissected with needle-tip electrocautery, leaving a thin layer of fat under the orbicularis and over the periosteum to create a glide aircraft to prevent restrictive adhesions. Dissection is continued in the preperiosteal plane into the world of the temporal fascia. The space for dissection is outlined, and dissection is carried out within the preperiosteal airplane to launch brow fixation points. C, An inner browpexy suture is positioned in the periosteum approximately 10 mm above the orbital rim. D, A suture is positioned in the deep temporal fascia to produce an upward and outward vector of fixation.
Syndromes
- Walking difficulties
- Sneezing
- Excessive bleeding
- Hydrocarbons (alkanes, cycloalkanes, aromatics)
- Lack of oxygen before or right after birth
- Tell your doctor about any cold, flu, fever, herpes breakout, or other illness you may have before your surgery.
Buy generic isoniazid 300mg
Inferior subperiosteal blind dissection is performed to roughly 2 cm above the supraorbital rim, remaining in a safe zone away from the frontal department of the facial nerve and the supraorbital and supratrochlear neurovascular bundles. Once the central subperiosteal cavity is dissected, the temporal incisions are made. Partial myectomy of the corrugators and procerus is performed to improve the glabellar areas. Care is required to prevent retraction damage to the frontal branch of the facial nerve. When the process is carried out by a right-handed surgeon, the facial nerve on the left facet is at threat of a traction injury by the endoscope. If the left frontal department undergoes excessive or prolonged upward traction by the endoscope, left frontal paresis can happen. Care is taken to stop injury to the supraorbital nerve, significantly if it exits via a bony foramen, the incidence of which is 15%. E, After an optical cavity is created, the endoscope is inserted through the central incision to facilitate using both lateral incision. G, A retracting sleeve, when inserted over the endoscope, increases the realm of retraction for visibility. Chapter 6 � Surgical Rejuvenation of the Forehead and Eyebrows 191 If the surgical procedure additionally entails a temporal incision, the dissection is carried out on the superficial layer of the deep temporal fascia posterior to the galea or the temporoparietal fascia. The sentinel vein is recognized and preserved or divided underneath direct visualization with electrocautery and endoscopic scissors, if needed for extra elevation. In the brow space, the periosteum is launched right down to the supraorbital rim, with cautious identification of the notch or foramen of the supraorbital or supratrochlear nerves. If a foramen exists, cautious periosteal launch to the supraorbital rim is crucial to forestall harm to or transection of the nerve. To decrease the danger of traction harm, the surgeon should be sure that the release of the periosteum is inferior to the frontal department of the facial nerve. This confirms that the surgeon is working inferior to the frontal branch, and the periosteum may be safely divided to release the forehead and brow for elevation, with out injuring the frontal nerve department. The transverse black line approximates the level of the frontal department of the facial nerve, which traverses the sphere above the level of dissection, and simply before one sees the sentinel vein, to innervate the frontalis on the deep lateral surface. A reverse periosteal dissector is used to stretch and unfold the periosteal incision alongside the supraorbital rim. The soft tissue is launched gently upward at or below the sentinel vein to stay inferior to the crossing branches of the frontal division of the facial nerve. Overcorrecting the nasal brow can produce an undesirable end result, with splaying of the brow and an increased, unnatural interbrow distance. However, if nasal brow elevation is needed, a whole midline launch of the periosteum is carried out. K, An endoscopic view exhibits the position of the reverse slicing periosteal elevator for incising the periosteum. M, the periosteum is launched on either facet and is vertically separated by incision and spreading. A partial myectomy is then undertaken in a transverse direction and working centrally, dividing a 1 to 2 cm strip of corrugator while preserving the supratrochlear nerve and vessels. These structures are commonly found passing through the physique of the corrugator muscle. Muscular ring�type compression has been reported as the cause of migraine headaches. This therapy has been helpful for treating migraine headaches by lowering the stress that acts because the pressure point. Additional launch of the depressor supercilii and procerus muscular tissues is carried out carefully to prevent overresection of the procerus, which can cause contour irregularity in the midline. All subcutaneous tissue should be preserved, and the myectomy ought to remove solely the muscle belly, thereby minimizing contour irregularities.
Isoniazid 300mg without prescription
Melanotic neuroectodermal tumor of infancy (melanotic progonoma) involving the calvaria. Khoddami M, Squire J, Zielenska M, et al: Melanotic neuroectodermal tumor of infancy: a molecular genetic examine. Nitta T, Endo T, Tsunoda A, et al: Melanotic neuroectodermal tumor of infancy: a molecular approach to diagnosis-case report. Shokry A, Briner J, Makek M: Malignant melanotic neuroectodermal tumor of infancy: a case report. Bonetti F, Pea M, Martignoni G, et al: the perivascular epithelioid cell and associated lesions. Bonetti F, Martignoni G, Colato C, et al: Abdominopelvic sarcoma of perivascular epithelioid cells. Jundt G, Moll C, Nidecker A, et al: Primary leiomyosarcoma of bone: report of eight cases. Kawai T, Suzuki M, Mukai M, et al: Primary leiomyosarcoma of bone: an immunohistochemical and ultrastructural examine. Lee E, Locker J, Nalesnik M, et al: the affiliation of EpsteinBarr virus with smooth muscle tumors occurring after organ transplantation. Gaffey M, Mills S, Askin F, et al: Clear cell tumor of the lung: a clinicopathologic, immunohistochemical, and ultrastructural examine of eight circumstances. Lantuejoul S, Isaac S, Pinel N, et al: Clear cell tumor of the lung: an immunohistochemical and ultrastructural research supporting a pericytic differentiation. Yamamoto H, Oda Y, Yao T, et al: Malignant perivascular epithelioid cell tumor of the colon: report of a case with molecular analysis. Takemori M, Nishimura R, Sugimura K, et al: Thoracic vertebral bone metastasis from uterine leiomyosarcoma. Lamovec J, Zidar A, Bracko M, et al: Primary bone sarcoma with rhabdomyosarcomatous element. Oda Y, Tsuneyoshi M, Hashimoto H, et al: Primary rhabdomyosarcoma of the iliac bone in an adult: a case mimicking fibrosarcoma. Mrad K, Sassi S, Smida M, et al: Osteosarcoma with rhabdomyosarcomatous component or so-called malignant mesenchymoma of bone. Van Dorpe J, Sciot R, Samson I, et al: Primary osteorhabdomyosarcoma (malignant mesenchymoma) of bone: a case report and evaluate of the literature. In 1913, Fischer17 described a peculiar tumor occurring predominantly in the tibia and infrequently in the fibula that was somewhat much like a extra common odontogenic adamantinoma of the jaw bones. Despite histologic similarity, there has been no proof that these tumors-of the jaw bone and of the lengthy bone-have an identical histogenetic origin. Adamantinoma of lengthy bones is extraordinarily uncommon; there are roughly 300 welldocumented cases printed in the world literature. The morphologic range of long bone adamantinomas also accounts for the persevering with controversy regarding their histogenesis. Another attention-grabbing phenomenon is the association of these tumors with areas resembling osteofibrous dysplasia (ossifying fibroma of long bones). The first description of areas of rarefaction related to long bone adamantinoma interpreted to be osteitis fibrosa was provided in 1942 by Dockerty and Myerding. The first comprehensive description of long bone adamantinoma associated with areas resembling fibrous dysplasia was offered in 1962 by Cohen et al. Therefore these authors have been the primary to postulate that, despite the histologic similarity to fibrous dysplasia, fibroosseous lesions related to adamantinoma may symbolize a distinctive characteristic related to these tumors. The description of ossifying fibroma of lengthy bone by Kempson38 in 1966 and the following redesignation of this lesion as osteofibrous dysplasia by Campanacci et al. Further studies of such composite lesions confirmed that the histologic and radiologic features of the fibroosseous elements had been more consistent with those of osteofibrous dysplasia. The second group is defined as differentiated adamantinoma and is characterised histologically by a predominance of an osteofibrous dysplasia�like pattern with a small, inconspicuous element of epithelial tumor elements. On radiographs, differentiated adamantinomas are intracortical and often multicentric lesions.
Order 300mg isoniazid amex
Gore-Tex implants have been initially popularized by Steinkogler for reconstructive eyelid surgery, and so they have been used efficiently as spacer materials for eyelid repair and for frontalis suspension associated to ptosis in place of fascia or silicone. The micropore matrix of polytetrafluoroethylene permits ingrowth of host fibrovascular tissue. Fibrovascular ingrowth occurs with minimal irritation, so the implant is properly tolerated. Local flaps could additionally be out there for this purpose; nevertheless, supplemental donor tissue grafts are commonly wanted. Autologous grafts suit this purpose greatest, particularly for sufferers who might have compromised healing, corresponding to those who have undergone multiple surgical procedures or irradiation. Some of these materials, including the extra present kinds of cross-linked collagen, have been described right here. A number of different grafts can be found, with the autologous types generally being most popular. An organized plan for lining, assist, and protection should be created, with emphasis on restoring eyelid function for opening and closing to shield the cornea along with reconstructing the lacrimal drainage system. The use and fate of fascia lata and sclera in ophthalmic plastic and reconstructive surgery. Reconstruction of the lateral canthus with trilobed pores and skin flap and temporalis fascia graft. Polytef (polytetrafluoroethylene) alloplastic grafting as a substitute for mucous membrane. Full-thickness lower eyelid reconstruction with a conchal chondro-perichondral graft and native protection with Mio-cutaneous flaps-our divisional expertise. Although these changes can range amongst people, there are several widespread causes of growing older, together with familial traits, loss of elasticity, sun damage, descent of periorbital tissue, and deflation of periorbital fats. The retaining ligaments of the periorbital area are fastened osteocutaneous ligaments, such because the orbitomalar ligament along the inferior orbital rim. Many of those aging adjustments can be corrected; we promote an anatomic method that makes use of surgical methods to restore a younger appearance. Brow-Forehead Changes As a person ages, the forehead has been historically thought to droop, and a forehead carry has been the benchmark for therapy of the upper face. However, longitudinal, nonlinear photographic studies by Lambros have proven that though the forehead could acquire wrinkles and drop, the aged eyebrow often strikes superiorly at the lateral forehead as a end result of the mix of deflation of soft tissue and the action of the brow elevator, the frontalis muscle. In many patients, nevertheless, significantly males with poor forehead support, the brow can also descend, which is obvious by a decrease within the resting brow-lash distance. B, A temporal lift is performed through a restricted incision with launch of the temporal line of fusion and the orbital retaining ligaments. B, this female affected person has good lateral brow position despite exercise of the frontalis muscle evident by the transverse brow rhytids and aging within the midface. Skin folding in the upper lid is brought on by both the loss of elasticity in the pores and skin itself and laxity and descent of the eyebrow. As many people age, the higher eyelid sulcus deepens, and they develop deep-set eyes. Upper lid curvature is determined by indentation from the spherical eyeball; as this indentation decreases, the curvature of the upper lid becomes much less pronounced. The pores and skin attachments of the aponeurosis generally remain intact, permitting retraction of the upper lid crease. Age can additionally be a contributing factor to one other involutional change that may happen within the levator aponeurosis-dehiscence of the medial horn, which causes lateral migration of the tarsal plate. Because the tarsal plate is now not centered on the pupil, this condition can cause flatness of the higher lid. Standard forehead laxity and descent must be addressed, however different potential causes have to be recognized. This fullness may be objectionable to patients, and repositioning the gland is typically needed.
Real Experiences: Customer Reviews on Isoniazid
Ur-Gosh, 33 years: Less incessantly, squamous cell carcinoma develops in the epithelialized lining of the bone defect.
Bozep, 43 years: A, T2-weighted magnetic resonance image exhibits intraspinal mass arising from synovium of cervical facet joint, which is affected by pigmented villonodular synovitis.
Dan, 55 years: Note focal attachment of lesion to floor of adjacent bone (left) and parallel periosteal new bone formation (arrows) on surface of adjacent bone (right).
Bram, 29 years: The sac may or is most likely not distended; nonetheless, regurgitation of mucus or pus again via the canaliculus and puncta is indicative of dacryocystitis and obstruction, both intermittent or everlasting, in the nasolacrimal duct or sac.
9 of 10 - Review by Q. Vandorn
Votes: 93 votes
Total customer reviews: 93
References
- Stacul F, van der Molen A, Reimer P, et al: Contrast induced nephropathy: updated ESUR Contrast Media Safety Committee guidelines, Eur Radiol 21(12):2527-2541, 2011.
- Salinas TJ, Eckert SE. In patients requiring single-tooth replacement, what are the outcomes of implant- as compared to tooth-supported restorations? Int J Oral Maxillofac Implants 2007;22(Suppl):71-95.
- Wilson RF, Christensen BV, Olivari MT, et al: Evidence for structural sympathetic reinnervation after orthotopic cardiac transplantation in humans, Circulation 83:1210, 1991.
- Moreland RB, Traish A, McMillin MA, et al: PGE1 suppresses the induction of collagen synthesis by transforming growth factor-beta 1 in human corpus cavernosum smooth muscle, J Urol 153(3 Pt 1):826n834, 1995.
- Safwat A, Leone BJ, Norris RM, et al: Pressure-length loop area: Its components analyzed during graded myocardial ischemia, J Am Coll Cardiol 17:790-796, 1991.
- Kusminsky RE: Complications of central venous catheterization. J Am Coll Surg 204:681-696, 2007.

