Retrovir dosages: 300 mg, 100 mg
Retrovir packs: 10 pills, 20 pills, 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Generic retrovir 100mg on line
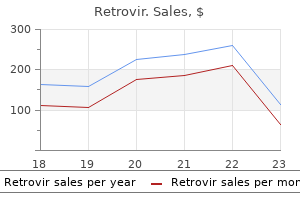
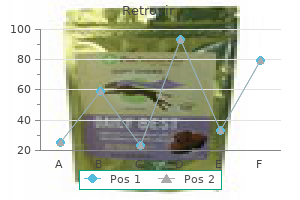
Radioimmunoassays have been used to precisely measure stavudine ranges in human subjects throughout a wide therapeutic range (Zhou et al. Serum levels of stavudine can be measured by a variety of other techniques, corresponding to reversed-phase high-performance liquid chromatography (Burger et al. There is appreciable affected person to affected person variation in plasma concentrations Table 229. There is equal distribution of stavudine between plasma and erythrocytes (Bristol-Myers Squibb, 2012). The central nervous system penetration of stavudine in mice is low, although a single oral dose of 25 mg/kg resulted in levels of stavudine in the mind of greater than zero. In humans, studies suggest that stavudine penetrates the cerebrospinal fluid to approximately the same extent as zidovudine (see Chapter 225, Zidovudine). However, a research looking at sufferers, most of whom had neurological illness, on mixture remedy discovered only 20% stavudine ranges when measured in opposition to plasma (Antinori et al. Ex vivo maternal�fetal placental switch research counsel that stavudine crosses the placenta by easy perfusion, quickly passing from the maternal to fetal circulation. There is a linear relationship between the mean focus of the drug within the fetal and maternal circulations (Bawdon et al. Stavudine is a low-molecular-weight compound and would be anticipated to be present in breast milk (Briggs et al. This approximate ratio was confirmed in a subsequent examine of fifty two ladies on combination treatment, with no stavudine detected in the infant (Fogel et al. Another examine showed an equal ratio between stavudine breast milk and plasma in ladies treated with stavudine, lamivudine, and nevirapine, once more with no transmission of stavudine to the breastfed toddler (Palombi et al. In a small research, seminal levels of stavudine in patients on mixture remedy had been discovered to be comparable or higher than that of plasma (Taylor et al. Clinically necessary pharmacokinetic and pharmacodynamic options There are few knowledge particularly correlating the pharmacokinetic and pharmacodynamic features of stavudine with its medical efficacy. The virologic efficacy of stavudine depends on the trough focus of the triphosphorylated form, stavudine triphosphate, throughout the cell. The frequency and severity of mitochondrial toxicity attributed to stavudine is dependent upon its dose and peak plasma focus (Domingo et al. Although additionally seen with zidovudine, zalcitabine, and didanosine, stavudine has been observed especially regularly to exhibit clinical toxicity as a end result of its profound effects on mitochondria. Alternative or additional mechanisms may also contribute, particularly altered expression of various metabolic genes (Mallon et al. While intensive research have documented stavudine toxicity, the massive move away from use of the drug in both creating and developed world situations, has meant that analysis has been displaced away from predictors or markers of toxicity, with the widespread availability of safer alternatives. Monitoring of surrogate markers for stavudine toxicity, notably lactate ranges, has been of some interest (Lonergan et al. Although hyperlactatemia is a extreme and recognized complication of stavudine remedy, delicate to moderate increases in serum lactate ranges have been proven to not be predictive of subsequent severe lactic acidosis (John et al. Renal clearance of stavudine is by both active tubular secretion and glomerular filtration. In vitro experiments utilizing isolated hepatocytes to assess the metabolic fate of stavudine demonstrated that stavudine is quickly cleaved to thymine, which is subsequently converted to beta-aminoisobutyric acid (Cretton et al. Simultaneous use of stavudine and didanosine is contraindicated due to the elevated frequency of mitochondrial toxicity. Co-prescription of stavudine and ribavirin has been associated with an elevated risk of mitochondrial toxicities, particularly lactic acidosis (Torriani et al. Co-prescription of agents identified to trigger peripheral neuropathy, particularly isoniazid and hydroxyurea, ought to be avoided because of their additive toxicity profiles. Fatal and extreme pancreatitis may develop when stavudine is taken in combination with hydroxyurea. In one other open-label, dose-ranging examine in a similar population, the incidence of peripheral neuropathy in sufferers receiving zero. Occurrence of peripheral neuropathy, by dose, throughout 96 weeks of stavudine treatment. This has been confirmed in quite a few studies within the mixture antiretroviral era, in both scientific trials and in massive observational trials (Hill et al.
Buy retrovir 100 mg otc
Hemorrhagic fever viruses as organic weapons: medical and public well being administration. Exposure of health care workers to ribavirin throughout therapy for respiratory syncytial virus infections. Severe migraine headaches are brought on by ribavirin but not by interferon alpha-2B together remedy for continual hepatitis C. Safety, tolerability, and pharmacokinetics of ribavirin in hepatitis C virus-infected patients with varied levels of renal impairment. A pilot research of combination remedy with ribavirin plus interferon alpha for interferon alpha-resistant persistent hepatitis C. In vitro inhibition of Chikungunya and Semliki Forest viruses replication by antiviral compounds: synergistic effect of interferon-alpha and ribavirin mixture. Effects of adding ribavirin to interferon to treat continual hepatitis C infection: A systematic review and metaanalysis of randomized trials. Ribavirin monotherapy for continual hepatitis C an infection: A Cochrane Hepato-Biliary Group systematic evaluate and meta-analysis of randomized trials. Effect of ribavirin in genotype 1 sufferers with hepatitis C responding to pegylated interferon alfa-2a plus ribavirin. Synthesis and characterization of a hemoglobin-ribavirin conjugate for targeted drug delivery. Dosage of ribavirin in patients with hepatitis C should be primarily based on renal perform: a inhabitants pharmacokinetic analysis. Interferon and ribavirin remedy in sufferers with hepatitis C-associated renal disease and renal insufficiency. Intravenous ribavirin therapy for adenovirus cystitis after allogeneic bone marrow transplantation. Assessing exposures of health-care personnel to aerosols of ribavirin-California. Fulminant adenovirus hepatitis following unrelated bone marrow transplantation: failure of intravenous ribavirin remedy. Parainfluenza virus type 3 infections in hematopoitic stem cell transplant recipients: response to ribavirin therapy. Pre-emptive oral ribavirin therapy of paramyxovirus infections after haematopoietic stem cell transplantation: a pilot study. Adenovirus infections following allogeneic stem cell transplantation: incidence and end result in relation to graft manipulation, immunosuppression, and immune recovery. Intravenous ribavirin for hantavirus pulmonary syndrome: security and tolerance throughout 1 year of open-label expertise. Acute pancreatitis associated with interferon and ribavirin therapy in patients with chronic hepatitis C. Aerosolized ribavirin-induced reversible hepatotoxicity in a hematopoietic stem cell transplant recipient with Hodgkin lymphoma. Adverse effects of ribavirin and outcome in extreme acute respiratory syndrome: expertise in two medical facilities. Ribavirin reveals a lethal threshold of allowable mutation frequency for Hantaan virus. Impact of ribavirin dose reduction throughout treatment in persistent hepatitis C genotype 1 sufferers. The function of ribavirin in direct acting antiviral drug regimens for chronic hepatitis C. Parainfluenza virus respiratory an infection after coronary heart transplantation: successful treatment with ribavirin. Comparative medical and laboratory analysis of the prophylactic capability of ribavirin, amantadine hydrochloride, and placebo in induced human influenza kind A. Fatal cardiomyopathy associated with pegylated interferon/ribavirin in a patient with continual hepatitis C.
Order 100mg retrovir with amex
The data from the trial, as a result of poor patient enrollment and untimely termination, are inadequate to assess main and secondary previously established end factors. Berhan and Berhan (2013) performed a meta-analysis of randomized managed clinical trials in drug-experienced sufferers handled with tipranavir�ritonavir or darunavir� ritonavir based mostly regimens. Tipranavir dose was 500 mg twice day by day and the twice-daily dose of ritonavir (100 or 200 mg) is shown within the table. At the 48-week end point, there were no significant differences among the three teams when it comes to virologic response (see Table 247. Further, there was no evidence of decreased responses to boosted tipranavir in sufferers contaminated with non-clade B virus, which was surprising provided that some non-B clades appeared to have a high background level of tipranavir-associated resistance mutations. Virologic failure charges had been similar across all three treatment groups, and not certainly one of the subjects analyzed had proof of genotypic resistance to tipranavir. However, treatment failures because of adverse event-related discontinuations had been significantly greater within the two tipranavir groups (100 and 200 mg ritonavir), 7. These variations had been largely because of more tipranavir-treated sufferers discontinuing therapy as a result of gastrointestinal adverse events (7 and eight patients, respectively, within the 100 and 200 mg ritonavir groups) compared to the lopinavir-treated patients (1 subject), and to elevations in liver transaminases (5 and 14 tipranavir-treated subjects compared to 2 topics treated with lopinavir). Based on the upper frequency of liver transaminase elevations in the subjects given tipranavir boosted with 200 mg of ritonavir, the exterior Data Safety Monitoring Board for this research recommended closure of this remedy group after the 48-week evaluation had been accomplished. In this research, sufferers had been randomized to obtain two totally different doses of tipranavir�ritonavir: excessive dose (375/150 mg/m3) or low dose (290/115 mg/m3). Both regimens were mixed with an optimized, nonprotease inhibitor, background routine. The one hundred fifteen antiretroviral-naive and -experienced pediatric sufferers enrolled within the research have been stratified by age group. Approximately half of the children had virus resistant to all protease inhibitors tested based mostly on genotype testing, > 80% had resistance to a number of nucleoside reverse transcriptase inhibitors, and 70% had virus immune to nonnucleoside reverse transcriptase inhibitors. This might have been as a end result of the younger patients had less antiretroviral experience (a median of three drugs in contrast with eight and 10 medicine, respectively, in older subjects) and fewer viral resistance as measured by genotypic sensitivity rating, median variety of protease gene mutations (10 in contrast with 13 and 17), and higher median tipranavir mutation scores (1. There was a development toward higher virologic response within the high-dose group in comparability with the low-dose group throughout all age groups (Salazar et al. The examine was extended up to 292 weeks to evaluate the long-term safety, efficacy, and tolerability of tipranavir� ritonavir. Among adolescents (12�18 years), 35/53 (66%) were receiving drug at week forty eight and 2/53 (4%) at week 288. Among patients 2 to < 6 years, 18/25 (72%) had viral hundreds < 400 copies/ml at week 48. Among older sufferers, week 48 responder charges had been 35% (13/37 of patients 6 to < 12 years) and 32% (17/53 of patients 12�18 years). By week 292, 6/37 (16%) of those 6 to < 12 years and 2/53 (4%) of those 12�18 years had viral masses < 400 copies/ml. Overall security and tolerability profiles had been finest for youngsters who initiated treatment between 2 and < 6 years (Salazar et al. Further, the drug has a quantity of unusual adverse reactions that deserve the attention of healthcare providers, including a propensity to trigger intracranial hemorrhage and severe and even deadly hepatitis. Increased risk of bleeding with the use of tipranavir boosted with ritonavir in haemophilic patients. Paper introduced at the fifth Conference on Retrovirusues and Opportunistic Infections, Chicago. Genotypic adjustments in human immunodeficiency virus type 1 protease related to decreased susceptibility and virologic response to the protease inhibitor tipranavir. Analysis of protease inhibitor combinations in vitro: activity of lopinavir, amprenavir and tipranavir 7d. Effects of boosted tipranavir and lopinavir on body composition, insulin sensitivity and adipocytokines in antiretroviral-naive adults. Steady-state disposition of the nonpeptidic protease inhibitor tipranavir when coadministered with ritonavir. The pharmacokinetics of single-dose and steady-state tipranavir/ritonavir 500 mg/200 mg in topics with mild or moderate hepatic impairment.
Buy retrovir 100mg without a prescription
Including kids switched from their initial routine, 82% of children in each groups had a viral load < 400 copies/ml after 4 years, with similar proportions amongst those originally handled with efavirenz (80%) and nevirapine (84%). Tolerability was related for the nonnucleoside and protease inhibitor teams but was not reported for the person brokers. Ninety-one kids had been randomized to obtain lopinavir�ritonavir and 92 to a nonnucleoside agent, 33 of whom have been treated with efavirenz and fifty nine with nevirapine. At week forty eight, the proportion of kids who achieved a viral load < four hundred copies/ml within the lopinavir�ritonavir arm (80%) was much like the nonnucleoside arm (76%), and the corresponding figures in the perprotocol analysis at week 96 had been 89% and 84%, respectively. A switch examine, much like these in adults (discussed later in this chapter), among 17 children on combination antiretroviral therapy with a nondetectable viral load who substituted a protease inhibitor for efavirenz reported only a single case of virologic failure (McComsey et al. Efavirenz was well tolerated, with no treatment-related discontinuations, no circumstances of rash, and 4 patients with self-limited nervous system symptoms. Smaller studies of efavirenz in kids, together with a nucleoside-sparing regimen of efavirenz plus lopinavir�ritonavir (Fraaij et al. Risk of virological failure at 2 years was lowest with a routine of three nucleoside agents and both efavirenz or nevirapine and was similar with the other regimens. Tolerability of all regimens was good, and remedy discontinuation charges at 5 years have been low and nonsignificantly different at 6. Efavirenz versus (or use in) regimens that are not really helpful Efavirenz has been in contrast with or included in regimens that are not utilized in medical follow and never beneficial in remedy guidelines; as such, the following data is included chiefly for historic interest. Before this examine, the mixture routine of zidovudine plus lamivudine plus indinavir was thought-about to be the antiretroviral regimen of alternative. At 48 weeks, outcomes of remedy were superior with efavirenz plus zidovudine plus lamivudine: virological efficacy was 70% with efavirenz plus zidovudine plus lamivudine, 48% with indinavir plus zidovudine plus lamivudine, and 53% with efavirenz plus indinavir. The remedy discontinuation price due to opposed events was higher with indinavir plus zidovudine plus lamivudine than with efavirenz plus zidovudine plus lamivudine. Superiority of efavirenz plus zidovudine plus lamivudine was maintained at week 168 (Tashima et al. A pharmacoeconomics study confirmed there was a considerable financial profit favoring the three-drug efavirenz regimen (Caro et al. This examine confirmed the superiority of zidovudine plus lamivudine plus efavirenz over different antiretroviral regimens in use at the time. Higher charges of virological suppression at 3 years, and lower charges of treatment discontinuation (overall and as a result of adverse events) had been noted in the three-drug efavirenz regimen. However, a scheduled review by the data security and monitoring board after a median of 32 weeks of followup led to a advice to stop the triple-nucleoside group. Patients on triple-nucleoside remedy have been subsequently offered openlabel efavirenz or the chance to participate in a substudy comparing addition of efavirenz with addition of tenofovir. A quadruple-nucleoside/nucleotide regimen of zidovudine plus lamivudine (or emtricitabine) plus abacavir plus tenofovir has been in contrast with two or three nucleoside/ nucleotides plus efavirenz in three studies (Moyle et al. As with remedy cohort research that examine efavirenz with protease inhibitors or nevirapine, results of similar research evaluating efavirenz with triple-nucleoside regimens (chiefly zidovudine plus lamivudine plus abacavir), are variable. The triple-nucleoside regimen was not inferior to zidovudine plus lamivudine plus efavirenz in a 24-month examine from France (Cuzin et al. A triple- or quadruple nucleoside (or nucleoside/nucleotide) regimen ought to be considered just for initial remedy under distinctive circumstances. These have been replaced by safer agents, similar to abacavir (see Chapter 230, Abacavir) and tenofovir (see Chapter 232, Tenofovir) and are not used extensively in high-income nations, so the mixture of efavirenz and a protease inhibitor ought to not often if ever have to be used these days. For the occasional affected person in whom it might be fascinating to use a nucleoside/nucleotidefree regimen for initial therapy. Rates of virologic suppression at 96 weeks with this routine (83%) differed little from those seen in patients assigned to the more standard efavirenz (89%) and lopinavir�ritonavir (77%) regimens (Riddler et al. However, increased lipid levels were extra frequent in these assigned to efavirenz plus lopinavir�ritonavir (Haubrich et al. The combination of efavirenz plus lopinavir�ritonavir was administered to sixty five treatment-naive and 21 treatmentexperienced sufferers in an open-label, noncomparative examine from France (Allavena et al.
Diseases
- Nonne Milroy disease
- Freire Maia odontotrichomelic syndrome
- Cleft palate
- Teebi Shaltout syndrome
- Chromosome 12, trisomy 12q
- Ankylosis
- Muscular phosphorylase kinase deficiency
- Microcoria, congenital
- Dysferlinopathy
Buy retrovir australia
Resistance was reported and analyzed phenotypically as well as genotypically, confirming the significance of lamivudine resistance along with mutations T184G, S202I, and/or M250V as a explanation for entecavir failure (Baldick et al. Some observational data counsel that that entecavir is associated with a decreased incidence of hepatocellular carcinoma and mortality in patients with cirrhosis (Hosaka et al. However, other research have nonetheless found a significant residual risk reinforcing the necessity for ongoing screening in patients with cirrhosis, significantly in patients of older age (Idilman et al. In a large Korean cohort study, entecavir, in comparison with lamivudine, was associated with a decreased mortality and danger of liver transplantation however had an identical threat of hepatocellular carcinoma (Lim et al. An ongoing area of clinical uncertainty are the indications to stop treatment with antiviral treatments. However, multiple research have proven a failure to maintain serological and virological responses after discontinuation of antiviral therapy in a high proportion of sufferers, and shut monitoring is required (Chaung et al. There are fewer studies evaluating entecavir with antivirals apart from lamivudine (see Table 254. Comparisons between entecavir and different antiviral brokers, including selected consequence measures. Comparator (number of patients) Follow up duration Surrogate outcomes Clinical outcomes Reference Country/region Population Clinical trials Entecavir (n = 354) vs. In a nonrandomized cohort examine comparing sufferers on entecavir with telbivudine, the next proportion of patients treated with entecavir had viral suppression (97% vs. Similar results have been reported in another cohort research comparing patients on entecavir with these on tenofovir and lamivudine. A greater proportion of patients receiving entecavir or tenofovir had viral suppression at 12 months, in comparability with those on lamivudine (93%, 92%, and 71% respectively) (Koklu et al. Although the high genetic barrier to resistance to entecavir has tempered enthusiasm for combination remedy, a selection of trials have been carried out (see Table 254. Because of twin activity in opposition to both viruses, tenofovir is often most well-liked as a half of a complete antiviral routine in such patients. A number of observational cohort research have instructed that entecavir is associated with viral suppression after liver transplant (Fung et al. However, antiviral remedy could also be considered in older adults with excessive stage viremia with histological proof of necroinflammation or fibrosis on biopsy (Terrault et al. The long-term effect of antiviral therapy in youngsters on medical end points such as 7f. Preemptive remedy before immunosuppression or chemotherapy Reactivation of hepatitis B after immunosuppression or chemotherapy is nicely acknowledged, particularly in association with using rituximab (Lok et al. A scientific trial has even demonstrated the prevalence of entecavir over lamivudine in patients with low viral masses (< 103 copies/ml) (Huang et al. While tips usually suggest antiviral prophylaxis for sufferers receiving immunosuppression, the 7. Clinical makes use of of the drug 4333 comparative cost-effectiveness of various antiviral brokers has not yet been established (Hwang et al. Comprehensive evaluation of hepatitis B virus reverse transcriptase substitutions related to entecavir resistance. Lack of pharmacokinetic interplay when entecavir is co-administerd with lamivudine, adefovir, or tenofovir and entecavir dosing with renal impairment. Paper offered on the fortieth Annual Meeting of the European Association for the Study of the Liver, Paris. A dose-ranging examine of the efficacy and tolerability of entecavir in lamivudine-refractory chronic hepatitis B sufferers. Long-term entecavir therapy ends in the reversal of fibrosis/cirrhosis and continued histological enchancment in sufferers with chronic hepatitis B. High genetic barrier nucleos(t)ide analogue(s) for prophylaxis from hepatitis B virus recurrence after liver transplantation: a scientific review. Long-term entecavir therapy leads to sustained antiviral efficacy and extended life span within the woodchuck mannequin of continual hepatitis infection. Nucleoside analogue can enhance the long-term prognosis of patients with hepatitis B virus infection-associated acute on continual liver failure. Safety and efficacy of oral entecavir given for 28 days in sufferers with persistent hepatitis B virus infection. Antiviral therapy of chronic hepatitis B virus infections: the past, the present and the future. Entecavir monotherapy is effective in suppressing hepatitis B virus after liver transplantation.
Order retrovir overnight delivery
Three cases of zidovudine-induced fever that was confirmed by rechallenge have been described, related in one case with IgM antibodies directed in opposition to a zidovudine serum protein conformational determinant (Jacobson et al. Hypertrichosis of the eyelashes has been reported inside 2 weeks of commencing zidovudine with out a rise in different physique hair size (Klutman and Hinthorn, 1991). Zidovudine administration in high doses to pregnant mice was associated with being pregnant failure in a single study (Toltzis et al. There is in vitro evidence of embryonic toxicity, resulting from failure to develop to the blastocyst stage when embryos are exposed to very excessive 3674 Zidovudine concentrations of zidovudine, however not with different nucleoside analogs, similar to didanosine (Toltzis et al. No discount in spermatogenesis or follicular improvement was seen in mice and rats receiving oral zidovudine (Sikka et al. However, in pigtailed macaques who received zidovudine throughout pregnancy, fetal development was normal, and there was no evidence of behavioral delay in infants (Ha et al. There was no proof of excess fetal or neonatal deaths, untimely labor, delayed fetal development, or extra congenital abnormalities attributable to zidovudine publicity. The hemoglobin focus was lower at delivery in infants exposed to zidovudine (mean difference between groups < 1 g/dl), however this difference had resolved by 12 weeks of age (Connor et al. Other available knowledge typically help the security of zidovudine use in pregnancy, though transient lactic acidosis is reported in neonates administered zidovudine chemoprophylaxis (Scalfaro et al. In a retrospective study of forty three pregnant girls who have been prescribed oral zidovudine in doses ranging from 300 to 1200 mg per day, the drug was well tolerated and never associated with teratogenic effects, even with publicity to zidovudine during the first trimester (Sperling et al. In a followup research of the offspring of seven pregnant women who have been prescribed 18 mg/kg zidovudine after the 16th week of gestation, all infants developed macrocytosis and two developed anemia, which in both cases resolved inside the second month of life (Ferrazin et al. Some of the out there human knowledge additionally point to mitochondrial dysfunction after perinatal use of this class of medication. No critical long-term toxicity from zidovudine was noticed by age 18 months, together with no toddler with symptoms suggestive of mitochondrial dysfunction and no malignancy within the zidovudine uncovered group (Chotpitayasunondh et al. Generally, zidovudine has been discovered to be safe in this context, regardless of a report of two circumstances of hepatotoxicity and rash occurring with mixed prophylactic use of zidovudine 7. Observation of 224 healthcare workers administered 1000 mg of zidovudine every day for 4�6 weeks in Italy discovered that > 50% experienced mild side effects, corresponding to nausea, malaise, fatigue, and headache, which led to drug cessation in 29 instances (13%). Subsequent observations of American healthcare staff confirmed that minor, reversible antagonistic effects, similar to nausea, malaise, fatigue, and headache, are skilled by up to 75% of people utilizing zidovudine monotherapy as postexposure prophylaxis, with associated zidovudine discontinuation rates > 30% (Tokars et al. More current statement of opposed occasions among people prescribed 28 days of mixture antiretroviral therapy for nonoccupational postexposure prophylaxis additionally discovered that zidovudine-based regimens had been associated with excessive rates of discontinuation of therapy (around 30%) as a outcome of side effects such as nausea, malaise, and headache (Winston et al. The serum level of zidovudine roughly 8 hours postingestion was 24 �g/ml (Spear et al. No scientific toxicity was observed in a 27-month-old boy who ingested one hundred thirty mg zidovudine (10. A f4-day-old toddler inadvertently given 10 times the beneficial dose of zidovudine for two days developed a metabolic acidosis that resolved inside 24 hours and neutropenia that endured for 5 weeks (Livshits et al. A brief evaluate of the main medical trials leading to current scientific use of zidovudine is supplied in the following sections (see Table 225. Most studies demonstrated a delay in disease progression with out long-term survival benefits in this context. This is according to current understanding of the rapid improvement of resistant viral strains (and therefore lack of sturdy remedy benefits) in sufferers utilizing antiretroviral monotherapy. Despite this, 42% reduction in mortality with didanosine and 32% with zalcitabine (vs. Viral load < four hundred copies/ml at 48 weeks in 70% (atazanavir) and 64% (efavirenz) Viral load < 400 copies/ml at 48 weeks in 51% in each arms, but within the subset with viral load > one hundred,000 copies/ml at baseline, those in the abacavir arm did poorly (viral load < four hundred copies/ml at forty eight weeks in just 31% vs. However, prolonged followup of the study cohort discovered no survival benefit associated with zidovudine remedy (Volberding et al. Of note, zidovudine use was related to a discount in high quality of life that approximated the advance in life quality derived from the delay in disease progression (Lenderking et al. This is also supported by observational information from a cohort of 936 asymptomatic sufferers in Italy (Vella et al. However, a scarcity of sustained profit, including an absence of improved survival, has also been confirmed in randomized, placebo-controlled trials (Anonymous, 1994; Mannucci et al. However, in 119 sufferers who had received 1�8 weeks of prior zidovudine exposure, there was no difference between zidovudine and didanosine. In the 118 sufferers who had acquired 8�16 weeks of prior zidovudine remedy, the 500-mg dose of didanosine was associated with much less illness development than zidovudine and the 750-mg dose of didanosine was associated with greater survival, although 2 sufferers on this arm died of pancreatitis.
Buy retrovir 100mg with mastercard
This group also advised that the dramatic decline in prevalence of pneumocystis pneumonia after combination antiretroviral remedy (following improvement of protease inhibitors) was because of the impact of protease inhibitors on P. As with different protease inhibitors, resistance to tipranavir develops slowly as a outcome of a number of mutations are required for high-level resistance. A mixture of six protease gene mutations, I13V, V32I, L33F, K45I, V82L, and I84V, was associated with a > 10-fold lower in tipranavir susceptibility (Doyon et al. Clinical trials have proven the superiority of ritonavirboosted tipranavir over comparator protease inhibitors in highly remedy experienced patients (see section 7, Clinical makes use of of the drug). Function of mutation Tipranavir-selected resistance mutations Accessory tipranavir mutations Tipranavir hypersusceptibility mutations Major protease inhibitor mutations not associated with tipranavir resistance Tipranavir chosen resistance mutations associated with vital resistance to other protease inhibitors Resistance mutation V82L/T, V321, 147V, 154V/A/M, 184V Most frequent: L33F/I Others: E35G, K43T, Q58E, T74P, N83D, L89V L241, 150V, 150L, I54L, L76V 150V/L, V82A/F, 154L, L90M, D30N, N88S, L76V, G48V V82L/T, 184V, 154M, L33F/I Source: Data compiled from Stanford University (2008), hivdb. However, tipranavir does share two major mutations, V82L/T and I84V, and one essential accessory mutation, L33F, with many of the different protease inhibitors. In vitro, the major protease inhibitor mutations selected by tipranavir are V32I, I54V, V82L and I84V (Doyon et al. The most frequent protease inhibitor mutations to emerge throughout ritonavir-boosted tipranavir salvage therapy in medical trials are V82L, V82T, I84V, and L33F (Naeger and Struble, 2007). The major protease inhibitor mutations I47V and I54A/M have also been associated with reduced susceptibility to tipranavir (Baxter et al. A distinctive set of 21 mutations at 16 protease codons was identified and includes L10V, I13V, K20M/ R/V, L33F, E35G, M36I, K43T M46L, I47V, I54A/M/V Q58E, H69K, T74P V82L/T, N83D, and I84V (Baxter et al. Patients with a baseline rating of zero or 1 responded best to salvage regimens that included tipranavir. Those with scores between 2 and seven had an intermediate response, and those with scores of eight or higher had little or no response (de Mendoza et al. Analysis of medical trial knowledge also discovered that subjects with more than five primary protease inhibitor mutations at baseline had inferior virologic response charges if enfuvirtide was not included within the salvage routine. Primary mutations were defined as any amino acid substitution at codons 30, 32, 36, 46, 47, 48, 50, 53, 54, 82, 84, 88, or ninety. A set of 21 mutations from the original rating plus five mutations associated with increased susceptibility to tipranavir have been included in the analysis. Nine mutations at six codons appeared to be the major contributors to tipranavir resistance: I47V, I54A/M/V, Q58E, T74P V82L/T, and N83D. Of note, the five mutations associated with hypersusceptibility to tipranavir (L24I, I50L/V, I54L and, L76V) have been found to be an important predictors of susceptibility to tipranavir. It is attention-grabbing that the resistance weights were introduced as combination of mutations. The ultimate weights were 74P, 82L/T, 83D and 47V (+4), 58E and 84V (+3), 36I, 43T and 54A/M/V (+2), 10V, 33F and 46L (+1), 24I and 76V (-2), 50L/V (-4), and 54L (-6). Tipranavir-weighted score susceptibility categories were defined as susceptible 3, partially susceptible > 3 however 10, and resistant 11. Using the exterior cohort knowledge (n = 150), the weighted rating was extremely associated with week 8 viral load reduction (p = 0. In addition, virologic response charges to tipranavir decreased when there were 5 or extra mutations to any protease inhibitor at baseline. Individuals who acquired tipranavir with out concomitant enfuvirtide who additionally had 5 or extra baseline protease inhibitor mutations started to lose the antiviral response between weeks 4 and eight, whereas these receiving enfuvirtide with tipranavir were able to obtain larger than 1. Site-directed mutagenesis has proven that the presence of six mutations in the protease coding sequence (I13V, V32I, L33F, K45I, V82L, and I84V) confer a higher than 10-fold reduction in susceptibility to tipranavir (Boehringer-Ingelheim, prescribing info, 2015). In vitro, resistant viral clones with > 10-fold resistance to tipranavir also confirmed decreased susceptibility to amprenavir, atazanavir, indinavir, lopinavir, nelfinavir, and ritonavir. Because ritonavir-boosted tipranavir has been studied as part of salvage remedy in extremely experienced patients, clinical data on mutation choice and impact in antiretroviral-naive individuals are missing. Mutations at six residues have been related to a decrease rate of virologic response (E35D/G/K/N, M36I/L/V, Q58E, Q61D/ E/G/H/N/R, H69I/K/N/Q/R/Y, and L89I/M/R/T/V), whereas one mutation (F53L/W/Y) was associated with the next rate of virologic response. The genotypic rating M36I/L/V - 53L/W/Y + Q58E + H69I/K/N/Q/R/Y + L89I/M/R/T/V was selected as indicating a powerful probability of a virologic response to ritonavir-boosted tipranavir. Of the seven sufferers with a genotypic score of -1 (viruses with only a codon fifty three mutation), all responded, and the proportions had been 79%, 56%, 33%, 21%, and 0% for those with genotype scores of 0, 1, 2, 3, and four, respectively. Most mutations associated with a failed virologic response to tipranavir had not previously been associated with protease resistance, in maintaining with phenotypic evaluation exhibiting that tipranavir has a singular resistance profile. They performed genotypic and phenotypic analyses of 39 matched patient samples at baseline and after tipranavir failure and found the bulk (84%) of isolates that had been prone to darunavir at baseline remained prone after virologic rebound on tipranavir-based therapy (Elston et al. Genotypes had been evaluated primarily based on the Stanford mutation score: sufferers were ranked for tipranavir and darunavir resistance and categorized as totally prone (class 1) or as having potential low-level resistance (2), definite low-level resistance (3), intermediate-level resistance (4), or high-level resistance (5).
Order discount retrovir on line
High-level resistance to (�) enantiomeric 2-deoxy-3-thiacytidine in vitro is as a outcome of of one amino acid substitution within the catalytic site of human immunodeficiency virus sort 1 reverse transcriptase. Pharmacodynamics of 2,3-dideoxycytidine: an inhibitor of human immunodeficiency virus. Phase 1 analysis of zalcitabine administered to human immunodeficiency virus-infected youngsters. The role of cytoplasmic deoxycytidine kinase in the mitochondrial effects of the antihuman immunodeficiency virus compound. Treatment of human immunodeficiency virus an infection with saquinavir, zidovudine and zalcitabine. In vitro choice of human immunodeficiency virus sort 1 immune to 3-azido-3-deoxythymidine. Synergistic inhibition of replication of human immunodeficiency virus kind 1, including that of a zidovudine-resistant isolate, by zidovudine and a couple of,3-dideoxycytidine in vitro. Ultrastructure of peripheral neuropathy induced in rabbits by 2,3-dideoxycytidine. Human immunodeficiency virus sort 1 pol gene mutations which trigger decreased susceptibility to 2,3-dideoxycytidine. Generation of drug-resistant variants of human immunodeficiency virus type 1 in vitro passage in increasing concentrations of 2-3-dideoxycytidine and a couple of,3-dideoxy3-thiacytidine. The similar mutation that encodes low-level human immunodeficiency virus type 1 resistance to 2,3dideoxyinosine and 2,3-dideoxycytidine confers high-level resistance to the (�) enantiomer of 2,3-dideoxy-3-thiacytidine. Multiple drug resistant mutants of feline immunodeficiency virus selected with 2,3-dideoxyinosine alone and together with 3-azido-3deoxythymidine. Mutated K65R recombinant reverse transcriptase of human immunodeficiency virus sort 1 shows diminished chain termination within the presence of 2,3-dideoxycytidine 5-triphosphate and different medicine. Identification of novel mutations that confer drug resistance within the human immunodeficiency virus polymerase gene. Novel mutation within the human immunodeficiency virus sort 1 reverse transcriptase gene that encodes cross-resistance to 2,3-dideoxycytidine. Deoxynucleoside phosphorylating enzymes in monkey and human tissues present nice similarities, whereas mouse deoxycytidine kinase has a unique substrate specificity. Feline leukemia virusinduced immunodeficiency syndrome in cats as a mannequin for evaluation of antiretroviral remedy. Selective inhibition of the reverse transcription of duck hepatitis B virus by binding of 2,3-dideoxyguanosine 5-triphosphate to the viral polymerase. High-level resistance to zidovudine but to not zalcitabine or didanosine in human immunodeficiency virus from children receiving antiretroviral remedy. Inhibition of bone marrow myelopoiesis and erythropoiesis in vitro by anti-retroviral nucleoside derivatives. Substrate specificity of human deoxycytidine kinase toward antiviral 2,3-dideoxynucleoside analogs. Novel mutation (V75T) in human immunodeficiency virus kind 1 reverse transcriptase confers resistance to 2,3didehydro-2,3-dideoxythymidine in cell culture. The inhibitory exercise of a peptide derivative towards the growth of simian immunodeficiency virus in C8166 cells. Pharmacological inhibition of in vitro infectivity of human T lymphotropic virus sort I. Didanosine and zidovudine resistance patterns in clinical isolates of human immunodeficiency virus kind 1 as decided by a replication endpoint concentration assay. Dermatologic issues related to administration of 2,3-dideoxycytidine in patients with human immunodeficiency virus infection. Combination remedy with zidovudine and dideoxycytidine in sufferers with superior human immunodeficiency virus infection. Intestinal absorption of dideoxynucleosides: Characterisation using a multiloop in situ method. A pilot examine of sequential therapy with zidovudine plus acyclovir, dideoxyinosine and dideoxycytidine in sufferers with severe human immunodeficiency virus an infection.
References
- Bell TM, Turner G, MacDonald A, et al. Type-3 adenovirus infection. Lancet. 1960;2:1327-1329.
- Walton SF, Oprescu FI: Immunology of scabies and translational outcomes: identifying the missing links, Curr Opin Infect Dis 26(2):116n122, 2013.
- Rich NM, Collins GJ Jr, McDonald PT, et al. Popliteal vascular entrapment. Arch Surg. 1979;114: 1377-1384.
- Socie G, Henry-Amar M, Bacigalupo A, et al. Malignant tumors occurring after treatment of aplastic anemia. European Bone Marrow Transplantation-Severe Aplastic Anaemia Working Party. N Engl J Med 1993;329(16):1152-57.