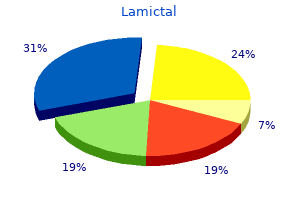
Lamictal dosages: 200 mg, 100 mg, 50 mg, 25 mg
Lamictal packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Order 25 mg lamictal overnight delivery
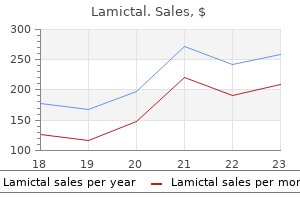
In the dose-response study, the reduction in median seizure rates was statistically significant for both higher dosage groups (32 mg and 56 mg) compared with the placebo group (43). Rash and psychosis occurred with approximately equal frequency in both groups (52). Neuropsychologic testing did not reveal any evidence of worsening in mood or cognitive abilities (53). Long-Term Studies No new adverse events occurred in long-term studies, nor were any additional severe adverse effects reported other than those already noted with short-term therapy (54). Of the eight patients who had visual symptoms, two had visual field defects from fixed lesions (temporal lobe resection, cortical infarct) and six had transient visual complaints. Color perception abnormality was seen in 7 of 17 patients and no contrast abnormalities were observed among the same 17 patients (95). Possible benefit for migraine (104), chronic pain (105), and primary insomnia (106,107) need to be confirmed with controlled studies. Dosages in children have not been well established; in one pediatric trial, doses 0. Routine monitoring of liver, renal, and bone marrow function does not appear to be necessary. Higher doses are well tolerated and appear to benefit some patients in open studies and in clinical experience. Tiagabine treatment is associated with neurochemical, immune and behavioural alterations in the olfactory bulbectomized rat model of depression. Antidystonic efficacy of gamma-aminobutyric acid uptake inhibitors in the dtsz mutant. Dose-dependent neuroprotection with tiagabine in a focal cerebral ischemia model in rat. Neuroprotective activity of tiagabine in a focal embolic model of cerebral ischemia. Neuroprotective effect of tiagabine in transient forebrain global ischemia: an in vivo microdialysis, behavioral, and histological study. The pharmacokinetic inter-relationship of tiagabine in blood, cerebrospinal fluid and brain extracellular fluid (frontal cortex and hippocampus). Role of the cytochrome P450 3A subfamily in the metabolism of [14C] tiagabine by human hepatic microsomes. Population analysis of the pharmacokinetics of tiagabine in patients with epilepsy. Pharmacokinetics of tiagabine, a gammaaminobutyric acid-uptake inhibitor, in healthy subjects after single and multiple doses. A randomised open-label study of tiagabine given two or three times daily in refractory epilepsy. A single-dose study to define tiagabine pharmacokinetics in pediatric patients with complex partial seizures. The pharmacokinetics of tiagabine in healthy elderly volunteers and elderly patients with epilepsy. Pharmacokinetics and safety of tiagabine in subjects with various degrees of hepatic function. An evaluation of the interaction between tiagabine and oral contraceptives in female volunteers. Adjunctive treatment of partial seizures with tiagabine: a placebo-controlled trial. Summary of five controlled trials with tiagabine as adjunctive treatment of patients with partial seizures. Tiagabine for complex partial seizures: a randomized, add-on, dose-response trial. A double-blind, placebocontrolled trial of tiagabine given three-times daily as add-on therapy for refractory partial seizures. Tiagabine as add-on therapy may be more effective with valproic acid-open label, multicentre study of patients with focal epilepsy. Efficacy and cognitive side effects of tiagabine and topiramate in patients with epilepsy. Meta-analysis and indirect comparisons of levetiracetam with other second-generation antiepileptic drugs in partial epilepsy. Open-label dosage and tolerability study of tiagabine monotherapy in patients with refractory complex partial seizures.
Purchase lamictal now
Dose to plasma concentrations are linear with low intra- and intersubject variability. Escalating dose administration orally results in near-linear increases in serum concentration. Lacosamide administered in a 300-mg single dose following consumption of a high fat diet did not influence its serum concentration. Distribution in placenta and breast milk and distribution in children has not been examined. A further 30% is metabolized by demethylation to the pharmacologically inactive O-desmethyl metabolite that is excreted in the urine (14). As a class, inducer antiepileptic medications increased clearance by approximately 36%. The observed effect of inducer antiepileptic medications on lacosamide exposure was modest. Accordingly, this finding is unlikely to be clinically significant when adding lacosamide to an existing treatment regimen. When used at therapeutic concentrations, lacosamide did not have a significant effect on the cytochrome P450 enzyme system. Human hepatocyte showed no potential to induce cytochrome P450 isoforms including 1A2, 2B6, 2C9, 2C19, and 3A4. The dosage at which this inhibition would be expected is unlikely to be routinely achieved in the treatment of human epilepsy. Generally, lacosamide was well tolerated when combined with up to three concomitant antiepileptic medications. Intravenous Administration Intravenous administration of lacosamide was studied in a multicenter, double-blind, double-dummy, randomized, inpatient trial evaluating the safety, tolerability, and pharmacokinetics as replacement for oral lacosamide (18). This study utilized patients from an open-label extension trial of oral lacosamide and randomized to either intravenous lacosamide and oral placebo or intravenous placebo and oral lacosamide. Treatment-emergent adverse events were mild and included dizziness, headache, back pain, somnolence, and injection site pain and were similar to oral lacosamide. There were no significant cardiac/hemodynamic adverse effects noted and there does not appear to be the need for special monitoring of cardiovascular function. Efficacy of the intravenous formulation in partial complex seizures or status epilepticus has not been studied. This is not surprising given the very recent availability of an intravenous formulation. Optimum effective dosage in adults is 200 to 400 mg/day suggesting similar type dosages for intravenous formulation. Case reports of usage in adults with status epilepticus have reported the use of 200 mg administered intravenously over 30 minutes with a subsequent repeat in 30 minutes. However, such recommendations need to be substantiated by carefully designed clinical studies. Signs of dose-related toxicity, typically seen with other antiepileptic medication-including ataxia, tremor, and reduced motility- occurred. This supratherapeutic effect was similar to that described for phenytoin, gabapentin, and carbamazepine. Clinical Adverse Effects Adverse events were evaluated in 944 subjects randomized to receive either lacosamide 200 mg/day (n 270), 400 mg/day (n 471), or 600 mg/day (n 203), or placebo (n 364) (17). Effects of the novel antiepileptic drug lacosamide on the development of amygdala kindling in rats. Acute and long-term effects of lacosamide in an animal model of status epilepticus. Lacosamide: an investigational drug for adjunctive treatment of partial-onset seizures. Efficacy and safety of oral lacosamide as adjunctive therapy in adults with partial-onset seizures.
Cheap lamictal 100 mg on-line
One study compared the efficacy and toxicity of phenytoin, phenobarbital, carbamazepine, and valproate as monotherapy in children with newly diagnosed epilepsy (131). Comparative efficacy was assessed by analysis of time to first seizure recurrence after the initiation of therapy, and by time to achieve a 1-year of seizure freedom. The likelihood ratio comparing the four drugs showed no difference between the drugs for either measure of efficacy at 1, 2, or 3 years of follow-up. Patients on phenobarbital were more likely to withdraw because of intolerable side effects, compared to those on the other drugs. There was no significant difference in the rate of withdrawal between the other drugs (131). Neonatal Seizures Phenytoin and phenobarbital monotherapy were compared in a randomized trial of 59 neonates with seizures confirmed by electroencephalography (132). Seizures were controlled in 43% of the phenobarbital group and in 45% of the phenytoin group. The authors concluded that both drugs were "equally but incompletely effective as anticonvulsants in neonates. As expected, the most common treatment for neonatal seizures was phenobarbital, which was given to 76% of all infants in the study (range, 56% to 89%, P 0. It was used to treat 16% of all neonates diagnosed with neonatal seizures (range, 8% to 36%, P 0. Phenytoin was started at least 1 day after phenobarbital 46% of the time, started on the same day as phenobarbital 32% of the time, and started at least 1 day before phenobarbital 11% of the time (133). The guideline concluded that based on available efficacy and effectiveness evidence alone, phenytoin and carbamazepine were efficacious or effective as initial monotherapy for adults with newly diagnosed or untreated partial-onset seizures (with the highest level of evidence, Level A). The findings in children was not that robust, and therefore, based on available efficacy and effectiveness evidence alone, phenytoin, carbamazepine, phenobarbital, topiramate, and valproate were possibly efficacious or effective as initial monotherapy for children with newly diagnosed or untreated partial-onset seizures (Level C). Some patients may experience prominent side effects at concentrations in the lower end of the therapeutic range, while others may be free of complaints despite elevated drug concentrations. Although small decreases may completely alleviate complaints, significant dose alterations may dramatically decrease serum concentrations, leading to a recurrence of seizures. Nausea, vomiting, and epigastric pain are often improved by dividing the dose or taking it with meals (or both). In general, however, effects appear modest when serum concentrations are kept within standard therapeutic ranges and polypharmacy is avoided (158,159). Unfortunately, patients taking phenytoin may suffer from cognitive side effects even when these guidelines are followed (160). In one study, phenytoin appeared to be associated with more cognitive effects than carbamazepine, although reanalysis excluding patients with elevated phenytoin concentrations showed no difference (161,168). When used as prophylaxis against seizures following head trauma, phenytoin demonstrated negative cognitive effects compared with placebo (169). No clinically significant difference in cognitive effects between phenytoin and valproate was detected in either healthy adults (170) or patients following craniotomy (140). In one study of elderly patients, phenytoin and valproic acid had similar effects (171), whereas a second study reported no cognitive impairment resulting from modest increases in serum phenytoin concentrations (between 11 g/mL and 16 g/mL) (172). Fluctuations in phenytoin serum concentrations by as much as 50% had no or an immeasurably small effect in children with well-controlled seizures receiving monotherapy with low therapeutic dosages (175).
Trusted 100 mg lamictal
Removal of the anterior temporal or inferior-basal language sites may explain this phenomenon (98). Other explanations include resection of cortex within 1 to 2 cm from essential language areas, brain retraction, and disruption of white matter pathways connecting language areas. According to Crandall and colleagues, persistent language disorders were found in three of 53 patients undergoing temporal lobe resection (99). In the Seattle series, removal of brain within 1 to 2 cm of essential sites established by intraoperative mapping was associated with mild language deficits (101,102). The "tailored operation" is designed to use languagemapping techniques to identify and protect neocortical language sites. Complications of Extratemporal Neocortical Focal Resections the extratemporal epilepsies considered for resective therapy are less frequent, more variable in their presentation, and the epileptogenic zone is more likely to involve eloquent cortex and intraoperative or extraoperative brain mapping is often necessary. All of these facts have a direct impact upon the complications of extratemporal neocortical focal resections, most important of which are the functional consequences of adequate removal of the epileptogenic zone in a particular brain area. In a systematic fashion, we can divide extratemporal focal resections in frontal, central, parietal, and occipital resections. Chapter 90: Outcome and Complications of Epilepsy Surgery 1017 Frontal Resections. The pattern of frontal language localization may be quite variable and many centers rely upon brain-mapping techniques to tailor frontal resections and avoid language complications. Transitory aphasic syndromes are often caused when resections are carried within 1 to 1. Long-lasting expressive aphasia can follow resection of language sites in the posterior inferior frontal gyrus or vascular compromise with postoperative ischemic injury to the region. Resections involving frontal cortex (superior frontal gyrus) may cause compromise of draining frontal veins with associated postoperative edema, venous infarction, as well as potential language and motor deficits. Functional studies have shown that this area is activated during initiation of movement and vocalization. Stimulation of this area leads to a fencing posture with bilateral motor movement. The orbitofrontal area is limited laterally by the orbitofrontal sulcus, medially by the olfactory sulcus, anteriorly and superiorly by the frontomarginal sulcus, and posteriorly by the anterior perforated area. The orbitofrontal cortex is extensively connected with the anterior and mesial temporal lobes, cingulum and opercular area, and for this reason, frequently misdiagnosed as anterior temporal seizures (107). On the nondominant side, extensive resection of the orbitofrontal cortex can be performed without deficits. The cognitive effects of extensive nondominant frontal resections are thought to be of minimal consequences in daily life activities (108). Furthermore, provided that a careful subpial technique is employed, with preservation of the vascular supply to motor cortex, frontal excisions may be safely carried up to the pial bank of the precentral gyrus. Care must be taken, however, not to undermine the motor cortex if the resections are extended into the white matter. Central type epilepsy or seizures arising from the primary motor and sensory area are infrequent. A more aggressive approach to the peri-Rolandic epilepsies is gaining acceptance in which extraoperative functional mapping of central cortex is supplemented by intraoperative remapping of this area by direct cortical stimulation, often under awake conditions. The partial resection of the nondominant face motor cortex may be safely performed, resulting in a transitory contralateral facial asymmetry. The superior resection margin should extend no higher than 2 to 3 mm below the lowest elicited thumb response. In the dominant hemisphere, some surgeons report postoperative dysarthrias and dysphasias following face motor cortex excision. The resection of the primary hand motor cortex produces a permanent deficit of fine motor control and should be avoided if useful hand function is present preoperatively. Resection of the primary leg motor cortex will elicit an immediate flaccid leg paralysis followed by gradual partial recovery of ambulatory capacity over months (97). Proximal limb function is likely to recover; however, distal ankle and foot permanent weakness are often present, requiring use of orthoses for safe ambulation. The resections of leg or face sensory cortex cause permanent but clinically insignificant deficit of proprioception in the leg or two-point discrimination in the lower face (109). In contrast, resection of hand sensory cortex is followed by important functional impairment, with the majority of patients showing deficits of pressure sensitivity, two-point discrimination, point localization, position sense, and tactual object recognition, which makes functional use of the involved hand difficult (109).
Purchase genuine lamictal on-line
The contents of the therapeutic class overviews on this website ("Content") are for informational purposes only. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Patients should always seek the advice of a physician or other qualified health provider with any questions regarding a medical condition. Clinicians should refer to the full prescribing information and published resources when making medical decisions. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults. This publication provides conclusions and a treatment algorithm based on a structured literature review of randomized trials of anticonvulsant treatments for seizures lasting longer than 5 minutes. Insufficient data exist in adults about the efficacy of levetiracetam as either initial or second therapy. No significant difference in effectiveness has been demonstrated between lorazepam and diazepam in adults with status epilepticus. Insufficient data exist in children about the efficacy of intranasal lorazepam, sublingual lorazepam, rectal lorazepam, valproic acid, levetiracetam, phenobarbital, and phenytoin as initial therapy. Insufficient data exist in children regarding the efficacy of phenytoin or levetiracetam as second therapy after failure of a benzodiazepine. Conclusions included the following (age not specified): Insufficient data exist about the comparative efficacy of phenytoin and fosphenytoin. When both are available, fosphenytoin is preferred based on tolerability, but phenytoin is an acceptable alternative. For prehospital settings or where first-line benzodiazepine options are not available, rectal diazepam, intranasal midazolam, and buccal midazolam are reasonable initial therapy alternatives. In the second phase of treatment (from 20 to 40 minutes after the beginning of the seizure), reasonable options include fosphenytoin, valproic acid, and levetiracetam. There is no clear evidence to guide therapy in the third phase of therapy (40 minutes after the beginning of the seizure). Guideline Development Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society (Go et al 2012). The literature review included an evaluation of 26 published articles on this topic. It is intended for internal use only and should be disseminated only to authorized recipients. The contents of the therapeutic class overviews on this website ("Content") are for informational purposes only. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Patients should always seek the advice of a physician or other qualified health provider with any questions regarding a medical condition. Clinicians should refer to the full prescribing information and published resources when making medical decisions. Evidence is insufficient to recommend other therapies (valproic acid, vitamin B6, nitrazepam [not available in the United States], levetiracetam, zonisamide, topiramate, the ketogenic diet, or novel/combination therapies) for treatment of infantile spasms. A shorter lag time to treatment of infantile spasms with either hormonal therapy or vigabatrin may be considered to improve long-term cognitive outcomes. There is a lack of sufficient randomized trials to provide definitive answers to key questions related to treatment of infantile spams. Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society (Hirtz et al 2003). The majority of children who experience a first unprovoked seizure will have few or no recurrences. Treatment has been shown in several studies combining both children and adults to reduce the risk of seizure recurrence; however, there is a relative paucity of data from studies involving only children after a first seizure. This publication recommends an approach to the standard and optimal management of infants with seizures. When possible, recommendations are evidence-based; however, when no evidence was available, recommendations are based on expert opinion and standard practice.
Discount lamictal on line
Effect of tiagabine on sleep in elderly subjects with primary insomnia: a randomized, double-blind, placebocontrolled study. Pharmacokinetic variability of newer antiepileptic drugs: when is monitoring needed Recurrent complex partial status epilepticus associated with tiagabine rechallenge. Nonconvulsive status epilepticus due to a de novo contralateral focus during tiagabine adjunctive therapy. Tiagabine-related non-convulsive status epilepticus in partial epilepsy: three case reports and a review of the literature. Two cases of nonconvulsive status epilepticus in association with tiagabine therapy. Provocation of non-convulsive status epilepticus by tiagabine in three adolescent patients. Non-convulsive status epilepticus in two patients receiving tiagabine add-on treatment. Tiagabine-induced generalised non convulsive status epilepticus in patients with lesional focal epilepsy. Non-convulsive status epilepticus induced by tiagabine in a patient with pseudoseizure. Tiagabine-induced nonconvulsive status epilepticus in an adolescent without epilepsy. Total percentage body weight changes during add-on therapy with tiagabine, carbamazepine and phenytoin. It was first synthesized in the 1950s as a potential tranquilizer, but unlike the related dicarbamate, meprobamate, it has no tranquilizing nor sedative action. An inhibitory effect on high-threshold, voltage-sensitive calcium currents was reported (19). Fluorofelbamate stopped seizures in the rat self-sustaining status epilepticus model; it also retarded the development of subsequent spontaneous seizures, which suggests an antiepileptogenic effect (23). Clearance in children is higher, with mean values 40% higher in children 2 to 12 years old in comparison to adults (30). The "presurgical" design was repeated as a monotherapy trial and further confirmed efficacy (37). Adjunctive open-label use reduced seizure frequency by 53% among 30 children aged 2 to 17 years (38). Atonic seizures (drop attacks) were reduced by 34% and all seizures by 19%, versus a 9% decrease and a 4% increase, respectively, with placebo. The primary endpoint was time to occurrence of the fourth seizure or 29 days, whichever came first. The valproate dose was a compromise between a placebo control, considered unsafe, and a full-dose active control, which could have reduced the chance of detecting a difference (36). It should be noted that 15 mg/kg/day is the recommended starting dose for valproate. Clinically significant interactions with phenytoin, carbamazepine, valproate, and phenobarbital have been established (Table 62. Weight loss is most likely over the first year of use, then weight tends to level off in most patients (57). In one open-label, add-on assessment, behavioral problems were the leading cause of discontinuation (57). The overall dropout rate caused by adverse effects in clinical trials was 12% (33). As expected with most drugs, this rate is higher in community practice-21% in one open-label series (57).
Generic lamictal 50mg with mastercard
In contrast, later studies from the same institution (31), identified the mesial temporal limbic structures, especially the amygdala, as the sites most frequently producing psychic phenomena, even in the absence of an electrical afterdischarge. Gloor (84) pointed to methodologic differences to account for the discrepant results: Penfield and colleagues (14,41) stimulated mainly the lateral neocortical surface intraoperatively, whereas Gloor et al. To reconcile these differences, Gloor (84) proposed a hypothesis based on the model of a neuronal network with reciprocal connections-in this case, between the limbic structures and the temporal isocortex. Psychic phenomena arising "from the activation of matrices in distributed neuronal networks" could presumably be elicited from different locations within the temporal lobe, including temporal isocortex and various limbic structures. Forced thinking refers to an awareness of intrusive stereotyped thoughts, fixation on, or crowding of thoughts. Penfield and Jasper (14) separated it from psychic auras and localized it to the frontal lobe. Cold shivering and associated piloerection as auras are usually experienced over diffuse or extended areas, but can be localized. It is probably not localized to a single cortical area, but seems most common in temporal lobe epilepsy (85,86). They are distinguished from the sometimes unpleasant superficial genital sensations without sexual content that arise from stimulation of the primary somatosensory area at the parasagittal convexity or interhemispheric fissure and possibly the perisylvian region. Sexual auras seem to arise most frequently from the temporal lobe (87) with other cases reported from the parasagittal area implicating the sensory cortex. Of those patients whose sexual aura resulted in orgasm, a right hemisphere lateralization has been found in one review (88). Epilepsy and Other Chronic Convulsive Diseases: Their Causes, Symptoms & Treatment. On right or leftsided spasm at the onset of epileptic paroxysms, and on crude sensation warnings, and elaborate states. Commission on Classification and Terminology of the International League against Epilepsy. Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Occipitotemporal epilepsy studied with stereotaxically implanted depth electrodes and successfully treated by temporal resection. The temporal sequence of aura-sensations in patients with complex focal seizures with particular attention to ictal aphasia. Mental phenomena evoked by electrical stimulation of the human hippocampal formation and amygdala. Correlative study of interictal electroencephalogram and aura in complex partial seizures. Epigastric sensations are considered an autonomic aura by some, although there is insufficient evidence for implication of autonomic afferent or efferent pathway activation. This can usually be verified by accompanying tachycardia on the electrocardiogram. Tachycardia of course occurs not just with the aura, but even more frequently in complex partial or generalized seizures. Respiratory symptoms experienced as an aura include such sensations as not being able to breathe, a need to breathe more deeply, and of a breath filling the chest that would not expire. Alterations in respiratory rhythms have been reported on stimulation of temporal limbic structures and in seizures of insular origin (53). Functional organization of supplementary motor cortex: evidence from electrical stimulation. Functional anatomy of the human supplementary sensorimotor area: results of extraoperative electrical stimulation. Case of tumour of the right temporosphenoidal lobe bearing on the localization of the sense of smell and on the interpretation of a particular variety of epilepsy. The abdominal aura: a study of abdominal sensations occurring in epilepsy produced by depth stimulation. Hemicrania epileptica: synchronous ipsilateral ictal headache with migraine features. A new type of epilepsy: benign partial epilepsy of childhood with occipital spike-waves. Longitudinal clinicoelectrophysiologic study of a case of Lafora disease proven by skin biopsy. Autonomic auras: left hemispheric predominance of epileptic generators of cold shivers and goose bumps
Discount lamictal online mastercard
In polytherapy, lamotrigine is particularly efficacious with valproate and this combination may be ideal for drug-resistant generalized epilepsies including those with myoclonic jerks. Usually, small doses of lamotrigine added to valproate may render previously intractable patients seizure-free. A metaanalysis of individual patient responses to lamotrigine or carbamazepine monotherapy. Drug interactions involving the new second- and third-generation antiepileptic drugs. Valproate effects on kinetics of lamotrigine in pregnancy and treatment with oral contraceptives. Antiepileptic drugs and hormonal contraceptives in adolescent women with epilepsy. It is also a likely candidate to replace valproate in the treatment of juvenile myoclonic epilepsy and of idiopathic generalized epilepsies in general. Because levetiracetam is associated with a relatively good safety profile, does not cause significant idiosyncratic reactions, has simple pharmacokinetic characteristics and has a low propensity to interact with other medications makes its clinical use straightforward and uncomplicated. Efficacy and tolerability of levetiracetam 3000 mg/d in patients with refractory partial seizures: a multicenter, doubleblind, responder-selected study evaluating monotherapy. Comparison of levetiracetam and controlled-release carbamazepine in newly diagnosed epilepsy. Drug interactions involving the new second- and third-generation antiepileptic drugs. Levetiracetam: pharmacology and therapeutics in the treatment of epilepsy and other neurological conditions. Levetiracetam reduces frequency and duration of epileptic activity in patients with refractory primary generalized epilepsy. Multicenter doubleblind, randomized, placebo-controlled trial of levetiracetam as add-on therapy in patients with refractory partial seizures. Open label, long-term, pragmatic study on levetiracetam in the treatment of juvenile myoclonic epilepsy. It has a high affinity for the benzodiazepine receptor so that its antiepileptic efficacy is similar to that of clonazepam. A very important potential advantage of lorazepam over diazepam is its longer duration of action, in both adults and children, and in neonates, where effects lasting 12 hours or more are usual. Lorazepam versus diazepam in the acute treatment of epileptic seizures and status epilepticus. Paradoxical precipitation of tonic seizures by lorazepam in a child with atypical absence seizures. Kinetic and dynamic study of intravenous lorazepam: comparison with intravenous diazepam. In contrast to ethosuximide, methsuximide has been reported to be effective as adjunctive therapy against partial seizures. Methsuximide lowers lamotrigine blood levels: a pharmacokinetic antiepileptic drug interaction. Methsuximide for complex partial seizures: efficacy, toxicity, clinical pharmacology, and drug interactions. Plasma levels of methsuximide and N-desmethylmethsuximide during methsuximide therapy. Midazolam is the only drug used in the management of status epilepticus which can be given by rectal administration or by intramuscular or intravenous injection. Its intramuscular use in premonitory status is a great advantage, and midazolam has an important clinical role at this stage in status as an alternative to intravenous or rectal diazepam.
Real Experiences: Customer Reviews on Lamictal
Hamlar, 39 years: Navigational Note: Urostomy leak Asymptomatic diagnostic Symptomatic; medical Severe symptoms; invasive finding; intervention not intervention indicated intervention indicated indicated Definition: A finding of leakage of contents from a urostomy. There is a large overlap between therapeutic, toxic and lethal cocaine concentrations and adverse reactions have been reported after prolonged use even with no measurable parent drug in the blood. Allopregnanolone is a potent, broad-spectrum anticonvulsant agent which is the active anticonvulsant progestin molecule in the diverse animal seizure models (35,41) as described above. In contrast to its effects in postpubertal rats, estrogen does not alter the rate of amygdala kindling in prepubertal male and female rats.
Muntasir, 60 years: This was the first gene mutation identified in association with an epilepsy syndrome. All lifetime costs were discounted by 3%, to derive the net present value of costs for 2019-20, which is $20. Pharmacokinetic variability of newer antiepileptic drugs: when is monitoring needed A range of 5 mg/L to 15 mg/L total may be more appropriate as a therapeutic range for the elderly (46).
Enzo, 61 years: Alternatives: for allergy, nasal saline, nasal steroid, 2nd generation antihistamine. Zopiclone has additional performance decrements when concurrently taken with alcohol, carbamazepine, and diazepam. Additionally, valproic acid use may cause life-threatening pancreatitis and is associated with impaired cognitive development and major congenital malformations (neural tube defects) limiting use in women of child-bearing age. Frameless image guidance can be used to place a 10-contact depth electrode through a rigid neuroendoscope within the atrium of the lateral ventricle.
Jaffar, 63 years: Transient mutism may be reduced by minimizing the retraction of frontal cortex and retracting the nondominant frontal lobe, if possible. Early surgical intervention may reduce this risk, but quantitative and prospectively collected data are scant. Seizures Manifested by Vocalization or Arrest of Vocalization Several types of utterances can occur during epileptic seizures. Patients should always seek the advice of a physician or other qualified health provider with any questions regarding a medical condition.
Eusebio, 59 years: Even then, however, one attempt at withdrawal may be reasonable as the prognosis may be more variable than previously thought (25,91). The maximum plasma level of creatine is reached less than 2 hours after the ingestion of doses of under 10 g, but after more than 3 hours for doses over 10 g, and may vary with the ingestion of carbohydrate, see food, page 157. Patients should maintain adequate hydration to increase urinary output and lower the concentration of stone-forming substances. Under certain unavoidable conditions, more restrictive filtering than that above may improve the recording.
Innostian, 50 years: The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Brain parenchymal oxygenation, cerebral blood flow, and brain glucose decrease all contribute to an energy mismatch (50). There have been reports of improvement in language, behavior, and seizure control in patients with Chapter 69: the Ketogenic Diet 795 acquired epileptic aphasia (59,60). Depending on the timing of dystonic pain, multiple different approaches may be helpful.
Hauke, 56 years: Other corticosteroids would be expected to interact similarly if given in adrenal-suppressant doses. Patients should always seek the advice of a physician or other qualified health provider with any questions regarding a medical condition. Substantial evidence from animal research and a growing number of studies in humans indicate that marijuana exposure during development can cause long-term or possibly permanent adverse changes in the brain. Conversely, abnormal levels of serum ammonia, carnitine, and fibrinogen, as well as hepatic function anomalies have been reported without clinically significant hepatotoxic reactions (45,72).
Bernado, 58 years: Febrile seizures are thus a genetically predetermined, age-dependent response to fever and not an epilepsy. Seizure frequencies were not reported, but were significantly reduced for the 400 mg/day (P 0. Ethosuximide88,6,109: A good relationship exists between drug dosage and plasma levels. I ended up going to multiple doctors to find help for my pain - orthopedists, physiatrists, a neurologist, and four top neurosurgeons.
10 of 10 - Review by C. Sancho
Votes: 313 votes
Total customer reviews: 313
References
- Gibbs CF, Johnson TM, Ouslander JG: Ofice management of geriatric urinary incontinence, Am J Med 120:211-220, 2007.
- Pohlmann R, Hasilik A, Cheng S, et al. Synthesis of lysosomal a-mannosidase in normal and mannosidosis fibroblasts. Biochem Biophys Res Commun 1983;115:1083.
- Wu AS, Trinh VT, Suki D, et al. A prospective randomized trial of perioperative seizure prophylaxis in patients with intraparenchymal brain tumors. J Neurosurg. 2013;118:873-883.
- Bluth RF, Carpenter HA, Pittelkow MR, Page DL, Coffey RJ. Immunolocalization of transforming growth factor-alpha in normal and diseased human gastric mucosa. Hum Pathol 1995; 26:1333.
- Maron BJ: Hypertrophic cardiomyopathy: A systematic review, JAMA 287:1308, 2002.

