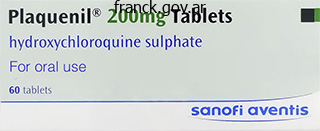
Plaquenil dosages: 400 mg, 200 mg
Plaquenil packs: 10 pills, 20 pills, 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Order plaquenil with a visa
The lower part of the anal canal, including the external haemorrhoidal venous plexus, drains by way of the inferior rectal branches of the internal pudendal vein into the interior iliac vein. The upper part surrounds the internal anal sphincter while the lowermost half encircles the anal canal inferior to the internal anal sphincter (Fritsch et al 2002, AlAli et al 2009). The upper a half of the external anal sphincter is attached to the ano coccygeal ligament posteriorly and to the perineal body anteriorly; some muscle fibres on each side of the sphincter decussate to type a commissure in the anterior and posterior midline. The uppermost fibres blend with the lower medial fibres of puborectalis and attach to the anococcygeal raphe posteriorly and the transverse perineal muscle tissue anteriorly. The decrease part of the exterior anal sphincter extends under the internal anal sphincter and is traversed by the terminal fibres of the conjoint longitudinal muscle (see above). Like the levator ani and inside anal sphincter, the exterior anal sphincter is tonically contracted at relaxation (the postural reflex). Within the area lie the intersphincteric anal glands, the supply of most anal fistulae (Parks 1961). There is an average of twelve intersphincteric anal glands inside the adult anal canal, evenly distrib uted around the circumference. Their perform is unknown, however they secrete mucin (different in composition from that secreted by rectal mucosa) and so they communicate with the anal lumen through ducts (lined by epithelium just like that of the anal transition zone), which cross the interior anal sphincter to open on the level of the anal valves imme diately above the dentate line (SeowChoen and Ho 1994). Retrograde passage of bacteria from the anal canal to the gland is understood to cause infection; inflammatory occlusion of the duct prevents spon taneous drainage again into the lumen of the anal canal. Sepsis may then unfold alongside a selection of routes to trigger abscesses and fistulae within various areas (Parks et al 1976). The arterial supply to the epithelium of the lower anal canal in the midline, significantly posteriorly, is comparatively deficient (Klosterhalfen et al 1989); this is further diminished if the interior anal sphincter is hypertonic (Schouten et al 1996). The epithelium is extra firmly teth ered to underlying constructions in the midline, which can also be a focus of stress in the anal canal. Collectively, these elements are thought to predispose to the occurrence of acute and persistent anal fis sures, which are mostly found in the midline, particularly posteriorly. They are associ ated with laxity of the anal canal submucosa and enlargement of the terminal branches of the superior rectal artery supplying the anal cushions. Lymphatic drainage Lymph from the upper anal canal drains cranially into the submucosal and intramural lymphatics of the rectum. Lymph from the decrease anal canal and external sphincter drains to inguinal lymph nodes. This sample of drainage is particularly necessary when contemplating lym phatic unfold of malignant tumours from the decrease rectum and anal canal. Blockage of lymph drainage alongside normal routes can result in unusual patterns of dissemination. It is influenced by a number of components, including colonic transit, stool volume and consistency, posture, age, gender, psychology and behaviour, culture and lifestyle (Palit et al 2012). Social behaviour entrains defecation to happen at a time of convenience somewhat than simply in response to a defecatory urge. The urge to defecate is pre ceded by highamplitude propagated contractions in the colon, which outcome in the antegrade propulsion of intraluminal contents to the rectum; these contractions increase in frequency and intensity simply before expulsion. The response to rectal filling entails intact rectal afferent nerves, reflex rectal contractions and normal rectal wall bio mechanics. The rectum acts as a reservoir and is ready to relax to accommodate faecal materials and fuel (adaptive relaxation). Periodic sampling within the upper anal canal helps to determine the nature of the rectal content material. If the defecatory urge is inconvenient, puborectalis and the external anal sphincter, that are tonically contracted at relaxation, may be further contracted voluntarily to transfer stool again up from the distal rectum. If the defecatory urge is associated with a conscious choice to evacuate, distal progression of colonic highamplitude propagating complexes, rectal contractions, raised intraabdominal stress from voluntary straining (the effectivity of which is influ enced by posture), relaxation of puborectalis (which straightens the anorectal angle) and the anal sphincters all mix to allow defeca tion. Relaxation of the internal anal sphincter is a reflex response to rectal distension, whereas leisure of the exterior anal sphincter is voluntary. During defecation, contraction of the conjoint longitudinal muscle shortens and opens the anal canal and flattens the anal cush ions. After defecation, the external anal sphincter contracts (the closing reflex), the interior anal sphincter progressively recovers its resting tone, and the postural reflex is reactivated.
Generic plaquenil 400mg overnight delivery
Naylor C, McCormack D, Sullivan S 1987 the midclavicular line: a wander ing landmark. Takazakura R, Takahashi M, Nitta N et al 2004 Diaphragmatic movement in the sitting and supine positions: healthy subject research using a vertically open magnetic resonance system. The pericardioperitoneal canals give rise to the pleural cavities surrounding the lungs and that a part of the peritoneal cavity surrounding the decrease finish of the foregut, which becomes the distal oesophagus, stomach and proximal duodenum. Later, these portions of peritoneal cavity are sequestered into the stomach cavity by the development of the diaphragm. In stage 14 embryos, the heart is on the level of the upper cervical somites and above the higher limb buds. The putative thoracic area incorporates the pericardial cavity ventrally and the pericardioperitoneal canals posteriorly, on both sides of the foregut. The future pleural cavities are as but undefined regions of the pericardioperitoneal canals. Below the guts, septum transversum mesenchyme is being invaginated by endodermal epithelial cells from the foregut hepatic primordium. The decrease partition of the thorax, the diaphragm, may be identified in stage 13 embryos; it migrates caudally consistent with the craniocaudal progression of improvement and the elongation of the neck. For the lungs to inflate and deflate, they should be surrounded by a whole pleural cavity barely bigger than the capability of the lungs. The synchronous development of the thoracic cage, diaphragm and pleural cavities is, therefore, of significant importance for the traditional improvement of the lungs and postnatal functioning of the respiratory system. These actions require an intact thoracic and stomach cavity, in order that the diaphragm can descend in direction of the rigid pelvic bowl, pushing out the belly wall. Other causes of interference with these actions embody neuromuscular problems of antenatal onset, corresponding to severe spinal muscular atrophy and myotonic dystrophy inherited from the mother, and lowered quantity of amniotic fluid. The lung buds are invested by splanchnopleuric mesenchyme derived from the medial partitions of the pericardioperitoneal canals, whereas the lateral walls produce somatopleuric mesenchyme, which contributes to the body wall. This latter mesenchyme is penetrated by the growing ribs, which arise from the thoracic sclerotomes. The future thoracic area lies caudal to the pharynx and extends to the higher a half of the septum transversum. Venous tributaries return blood from the physique, yolk sac and placenta, and arterial trunks pass each side of the pharynx. C, the respiratory diverticulum arises within the midline from the lower portion of the pharynx, and lung buds prolong dorsally into the pericardioperitoneal canals. The respiratory diverticulum arises from the ventral facet of the pharynx and grows caudally. Bilateral lung buds prolong dorsally into the pericardioperitoneal canals dorsolaterally. Later modifications in place of the frequent cardinal veins contribute to the formation of the pericardiopleural membranes cranial to the creating lungs, whereas folds of coelomic epithelium, pleuroperitoneal membranes, separate the pleural cavities from the peritoneal cavity. The bony and cartilaginous cage supplies insertions for the intercostal muscle tissue, which arise from the ventrolateral fringe of the epithelial plate of the somites. The somatopleuric coelomic epithelium, after its proliferative section, contributes to the mesothelium of the parietal layer of pleura. The communications with the pericardial and peritoneal coeloms turn out to be termed the pleuropericardial and pleuroperitoneal canals, respectively. In early embryos, the cavities retain substantial volumes of fluid and their walls are separate; they provide the route for a primitive type of circulation until superseded by the blood vascular system. In later fetal and postnatal life, the cavity walls are coapted, so that a mere microscopic film of serous fluid intervenes between them. A curved elevation of tissue, the pulmonary ridge, develops on the lateral wall of the pleural coelom and partly encircles the pleuropericardial canal. The creating lung bud abuts on the ridge, which, consequently, divides into two diverging membranes meeting at the septum transversum. As the apical part of the lung types, it invades and splits the body wall, and extends cranially on the lateral side of the common cardinal vein, preceded by an extension from the primary pleural coelom to kind a half of the secondary, definitive, pleural sac. In this fashion, the common cardinal vein and the phrenic nerve come to lie medially in the mediastinum.

Purchase plaquenil with mastercard
Note the aggregations of lymphocytes (blue) and undifferentiated epithelial cells (white). Key references Sphincteric causes of faecal incontinence may be structural (disrup tion or atrophy of a part of the sphincter musculature) or neuropathic (damage to the nerve provide to the sphincters), or a mix of both. The commonest causes of sphincter disruption are obstetric harm, anal surgery (for haemorrhoids, fistula or fissure) and trauma. Pudendal neuropathy is most commonly related to childbirth (prolonged second stage) and chronic straining. Although the anus constitutes the final barrier to faecal inconti nence, suprasphincteric components are also essential in sustaining faecal continence, significantly the speed at which the stool is delivered to the rectum, rectal sensation and compliance, and adaptive leisure. Conversely, continual rectal distension with retained faeces may lead to passive (overflow) leakage, possibly because of a chronically relaxed internal anal sphincter consequent on a persistently activated rectoanal inhibitory reflex, along with blunted rectal sensa tion causing diminished acutely aware contraction of the external anal sphincter. The unique description of the mesorectal plane and its relevance to the surgical excision of rectal tumours. A detailed postmortem angiographic examine demonstrating the arrangement of anal arterial provide. An anatomical and medical examine directed at understanding the character of haemorrhoids. It is thicker, darker, extra vascular, and extra loosely hooked up to the submucosa within the rectum. Lamina propria Epithelium the luminal floor of all however the anorectal junction is lined by colum nar cells, mucous (goblet) cells and occasional microfold (M) cells that are restricted to the epithelium overlying lymphoid follicles. The lamina propria is composed of connective tissue that supports the epithelium, forming a specialized pericryptal myofibroblast sheath round each intestinal gland. Solitary lymphoid follicles within the lamina propria, just like those of the small intestine, are most abun dant within the caecum, appendix and rectum, but are additionally current scattered along the the rest of the large intestine; efferent lymphatic vessels originate inside them. Columnar (absorptive) cells Columnar (absorptive) cells are probably the most quite a few of the epithelial cell types. Typical junctional complexes around their apices restrict extracellular diffusion from the lumen throughout the gut wall. Muscularis mucosae Submucosa the muscularis mucosae of the massive intestine is actually just like that of the small intestine. Muscularis externa the muscularis externa has outer longitudinal and inside round layers of clean muscle. Between the taeniae coli, the longitudinal layer is much thinner, less than half the thickness of the round layer. The round fibres constitute a skinny layer over the caecum and colon, and a thicker layer within the walls of the rectum; they type the interior anal sphincter within the anal canal. Interchange of fascicles between circu lar and longitudinal layers happens, particularly near the taeniae coli. Deviation of longitudinal fibres from the taeniae coli to the round layer could, in some instances, clarify the haustrations of the colon. The glands are lined by low columnar epithelial cells, mainly goblet cells, augmented by columnar absorptive cells and neuroendocrine cells. The latter are situated mainly on the bases of the glands, and secrete basally into the lamina propria. Stem cells located at or near the bases of the intestinal glands (crypts) are the source of the opposite epithelial cell types in the giant intestine. They provide cells that migrate towards the luminal floor of the intestine; their progeny differentiate, endure apoptosis and are shed after roughly 5 days. Small, fatfilled appendices epiploicae are most numerous on the sigmoid and trans verse colon but generally absent from the rectum. AlAli S, Blyth P, Beatty S et al 2009 Correlation between gross anatomical topography, sectional sheet plastination, microscopic anatomy and endoanal sonography of the anal sphincter complex in human males. Bell S, Sasaki J, Sinclair G et al 2009 Understanding the anatomy of lym phatic drainage and the utilization of bluedye mapping to decide the extent of lymphadenectomy in rectal cancer surgery: unresolved points. A up to date evaluate of the neuroanatomy and physiology of colorectal motor perform.

Generic 400 mg plaquenil with mastercard
Usually, gravity alone is sufficient; when necessary, the lowest part of serratus anterior and pectoralis minor are active depressors. Vascular provide the acromioclavicular joint receives its arterial provide from branches of the suprascapular and thoracoacromial arteries. Innervation the acromioclavicular joint is innervated by branches from the suprascapular and lateral pectoral nerves. It has been suggested that the density of nociceptors is greatest within the inferior acromioclavicu lar ligament and capsule. Factors sustaining stability the acromioclavicular ligaments present the best resistance to anteroposterior displacement of the acromioclavicular joint, while the coracoclavicular ligaments resist rota tion and vertical translation of the joint. The sternal end of the clavicle is robustly supported by sturdy ligaments, and an identical, but less strong, association of ligaments suspends the scapula from the lateral end of the bone. The motion of the acromioclavicular joint is proscribed by its small surface area and the articular capsule. Protraction and retraction Protraction (forward movement) around the thoracic wall happens in pushing, thrusting and reaching movements, normally with some lateral rotation. The lateral (acromial) finish of the clavicle describes an asymmetric conical path throughout movement of the higher extremity. The maximal vary of rotation of the clavicle (subtended by the sternoclavicular joint) is 30�; the maximal vary of rotation of the scapula (sternoclavicular and acromioclavicular joints combined) is about 60� with respect to the sternum. Arguably, the ligaments may be better 10 defined as the claviculocoracoid ligaments, to acknowledge their function because the spiroid fulcrum round which the physique of the scapula, and subsequently the glenoid fossa, rotate during protraction and retraction of the scapula. The action of subclavius is to resist upward displacement of the distal clavicle, or to decelerate the clavicle transferring into elevation. The antagonist of trapezial energy is pectoralis minor, which, hardly ever, has an extension or slip of tendon that joins the coraco-acromial ligament. Shortening or tightness of pectoralis minor will create fixed protraction of the scapula, which then rotates ventrally around the chest wall. As a consequence, the acromion tilts and the area between it and the cranial surface of the rotator cuff beneath (the subacromial space) diminishes, creating the conditions in which forceful coaptation of the apposed surface of the rotator cuff and the coraco-acromial ligament might occur. Coraco-acromial ligament Coracoclavicular ligament Subclavius Pectoralis minor over the sternal facet, carrying the disc with it. Pectoralis major, together with the anterior sternoclavicular ligament and posterior lamina of the costoclavicular ligament, examine backward slide of the sternal end. Ser ratus anterior and pectoralis minor are prime movers and maintain continuous apposition of the scapula, particularly its medial border, in smooth gliding on the thoracic wall, with the rhomboid muscular tissues con trolling the rate and vary of movement. The upper part of latissimus dorsi also acts like a strap throughout the inferior scapular angle in protraction and lateral rotation. This motion is all the time associ ated with humeral elevation and rotation at the glenohumeral joint, and with protraction of the scapula. The acromioclavicular joint strikes within the first 30� of abduction, when the conoid ligament turns into taut, and is subsequently accompanied by clavicular rotation on the sternoclavicular joint across the longitu dinal axis of the bone. Some acromioclavicular motion additionally occurs in the final stages of humeral abduction. Trapezius (cervical fibres) and serratus anterior (the decrease part) are prime movers, with the rhomboids providing resistance to movement. Medial (downward) rotation is normally effected by gravity; gradual active lengthening of trapezius and serratus anterior is sufficient to management it. When more pressure is needed, levator scapulae, the rhomboids and, in the preliminary stages, pectoralis minor are prime movers in returning the scapula to a position of relaxation. Articulating surfaces the articular surfaces are reciprocally curved and are accurately termed ovoids. Both articular surfaces are coated by hyaline cartilage, thickest centrally and thinner peripherally over the humerus, and vice versa over the glenoid cavity. Glenoid labrum the glenoid labrum is a fibrocartilaginous rim around the glenoid fossa. The attachment to the sting of the glenoid fossa is safe superiorly where it blends with the anterior and posterior fasciculi of the lengthy tendon of biceps (Vangsness et al 1994), much less safe posteriorly, however comparatively more secure anteroinferi orly (Bankart 1923). There could also be an aperture between the free deep edge of the labrum and the anterior glenoid rim above the midpoint of the fossa.
Cheap plaquenil line
A motor speaking branch between the median and ulnar nerves in the forearm happens in approximately one-quarter of patients. The commonest variant has a branch passing from the anterior interosseous to the ulnar nerve. A variety of patterns have been described the place branches move between flexors digitorum superficialis and profundus, deep to the ulnar artery, to be a part of the ulnar nerve; such branches could explain the variations in innervation of the intrinsic muscle tissue. It provides off articular branches to the elbow as it lies between the medial epicondyle and the olecranon. The ulnar nerve enters the forearm between the 2 heads of flexor carpi ulnaris, which it supplies by two neurovascular pedicles: one arising just distal to the cubital tunnel and one in the forearm. It is superficial to the posterior and oblique elements of the ulnar collateral ligament. In the higher third of the forearm, the nerve is distant from the ulnar artery but, extra distally, it involves lie close to the medial aspect of the artery. Posterior interosseous nerve Branches in the forearm muscular branches There are two main muscular branches of the ulnar nerve within the forearm. They come up near the elbow and supply flexor carpi ulnaris and the medial half of flexor digitorum profundus. It perforates the deep fascia and descends alongside the medial side of the back of the wrist and hand. It provides supinator both earlier than entering the muscle and as it passes via it. As it emerges from supinator posteriorly, the nerve gives off three brief branches to extensor digitorum, extensor digiti minimi and extensor carpi ulnaris, and two longer branches: a medial branch to extensor pollicis longus and extensor indicis, and a lateral department that provides abductor pollicis longus and extensor pollicis brevis. The nerve at first lies between the superficial and deep extensor muscular tissues, however on the distal border of extensor pollicis brevis, it passes deep to extensor pollicis longus and, diminished to a fine thread, descends on the interosseous membrane to the dorsum of the carpus. Filaments arising from its flattened termination provide the carpal ligaments and articulations. Articular branches from the posterior interosseous nerve supply carpal, distal radio-ulnar and some intercarpal and intermetacarpal joints. Digital branches provide the metacarpophalangeal and proximal interphalangeal joints. Radial nerve compression Palmar cutaneous department the palmar cutaneous branch of the ulnar nerve arises in mid-forearm, descends on the ulnar artery, which it supplies, and then perforates the deep fascia. It communicates with the palmar department of the median nerve and ends in the palmar pores and skin. The most proximal of these is throughout the radial tunnel at the stage of the radial head, the place fibrous bands may be current. More distally, it has been instructed that branches of the radial recurrent artery might compress the posterior interosseous nerve. Other websites of compression are the tendinous edge of the deep floor of extensor carpi radialis brevis and the point at which the nerve passes beneath the arcade of Frohse and between the 2 heads of supinator. Rarely, the nerve could additionally be compressed on the stage of the distal border of supinator. It is most frequently compressed on the stage of the cubital tunnel; that is the most typical nerve compression syndrome after that of the median nerve within the carpal tunnel. Lateral cutaneous nerve of the forearm the lateral cutaneous nerve of the forearm is the cutaneous division of the musculocutaneous nerve (p. Its trunk gives rise to a slender recurrent department that extends alongside the cephalic vein as far as the center third of the upper arm, distributing filaments to the skin over the distal third of the anterolateral floor of the upper arm near the vein. At the wrist joint, the lateral cutaneous nerve of the forearm is anterior to the radial artery. It gives off filaments that pierce the deep fascia and accompany the artery to the dorsum of the carpus. The nerve then passes to the bottom of the thenar eminence, the place it ends in cutaneous rami, a few of which join with the terminal department of the radial nerve and the palmar cutaneous department of the median nerve. These branches arise from the primary radial nerve because it runs between brachialis and brachioradialis. The radial nerve divides into the posterior interosseous and superficial radial nerves anterior to the elbow on the stage of the tip of the lateral epicondyle. There is some variation within the stage at which branches of the radial nerve come up from the main trunk in several individuals. Branches to extensor carpi radialis brevis and supinator might arise from the primary trunk of the radial nerve or from the proximal a part of the posterior interosseous nerve, however almost invariably above the arcade of Frohse.
Generic plaquenil 200 mg online
Innervation Serratus anterior is innervated by the lengthy thoracic nerve, C5, 6 and seven, which descends on the external floor of the muscle. Actions With pectoralis minor, serratus anterior protracts (draws for wards) the scapula, as a main mover in all reaching and pushing transfer ments. The upper part, with levator scapulae and the upper fibres of trapezius, suspends the scapula; only slight activity is sufficient to support the unloaded arm. In the initial levels of abduction, serratus anterior helps other muscles to fix the scapula, so that deltoid acts successfully on the humerus and not the scapula. While deltoid is elevating the arm to a right angle with the scapula, serratus anterior and trapezius are simul taneously rotating the scapula; the mix permits the arm to be raised to the vertical. To effect this upward rotation of the scapula, ahead pull on the inferior angle by the lower digitations of serratus anterior is coupled with an upward and medial pull on the lateral end of the clavicle and acromion by the higher fibres of trapezius, and a downward pull on the bottom of the scapular backbone by the lower fibres of trapezius. Conversely, slow downward scapular rotation, assisted by gravity, is achieved by controlled lengthening of these muscles. More highly effective downward rotation requires balanced contraction of the upper fibres of serratus anterior, levator scapulae, rhomboids, pectoralis minor and the center a part of trapezius. When weights are carried in entrance of the physique, serratus anterior prevents backward rotation of the scapula. It arises from the anterior surface of the sternal half of the clavicle (clavicular head); half the breadth of the anterior floor of the sternum down to the extent of the sixth or seventh costal cartilage (sternal head); the primary to the seventh costal cartilages (first and seventh typically omitted); the sternal finish of the sixth rib; and the aponeurosis of external indirect (rectus head). The clavicular fibres are usually sepa rated from the sternal fibres by a slight cleft. The thicker anterior lamina is formed by fibres from the manu brium, joined superficially by clavicular fibres and deeply by fibres from the sternal margin and the second to fifth costal cartilages. The pos terior lamina receives fibres from the sixth (and, typically, seventh) costal cartilages, sixth rib, sternum, and aponeurosis of external indirect. Fibres from the sternum and aponeurosis curve around the lower border, turning successively behind these above them, which implies that this part of the muscle is twisted in order that the fibres which may be lowest at their medial origin are highest at their attachment on the humerus. The posterior lamina reaches larger on the humerus than the anterior, and offers off an growth that covers the intertubercular sulcus and blends with the capsular ligament of the shoulder joint. An expansion from the deepest a part of the lamina lines the intertubercular sulcus at its linear insertion; another growth descends from its decrease border into the deep fascia of the upper arm. The rounded lower border of pectoralis major forms the anterior axillary fold and turns into conspicuous in abduction against resistance. Variants the abdominal slip from the aponeurosis of external oblique is sometimes absent. The variety of costal attachments and the extent to which the clavicular and costal elements are separated range. A superficial vertical slip, or slips, might ascend from the lower costal cartilages and rectus sheath to blend with sternocleidomastoid or to attach to the upper sternum or costal cartilages. The intermediate part is multipennate; 4 intramuscular septa descend from the acromion to interdigitate with three septa ascending from the deltoid tubercle. The septa are connected by brief muscle fibres that present powerful traction (Leijnse et al 2008). The muscle surrounds the glenohumeral articulation on all sides, except inferomedially, giving the shoulder its rounded profile. The tendon offers off an enlargement into the brachial deep fascia that will reach the forearm. Variants Deltoid could fuse with pectoralis major or may receive addi tional slips from trapezius, the infraspinous fascia or the lateral scapular border. Teres minor shares a standard innervation and might be con sidered as a fourth, posteroinferior, part of deltoid. Relations the pores and skin, superficial and deep fasciae, platysma, lateral supraclavicular and upper lateral brachial cutaneous nerves are all superficial. The coracoid course of, coracoacromial ligament, subacro mial bursa, tendons of pectoralis minor, coracobrachialis, each heads of biceps brachii, pectoralis major, subscapularis, supraspinatus, infra spinatus, teres minor, lengthy and lateral heads of triceps, circumflex humeral vessels, axillary nerve, and the surgical neck and upper shaft of the humerus, together with both tubercles, are all deep. The anterior border of deltoid is separated from pectoralis main proximally by the infraclavicular fossa, which accommodates the cephalic vein and deltoid branches of the thoracoacromial artery; distally, these muscle tissue are involved. Deltoid Relations Skin, superficial fascia, platysma, medial and intermediate supraclavicular nerves, breast tissue and deep fascia are all anterior.
Cheap plaquenil 200mg online
The greater omentum typically extends from its attachment to the transverse colon on to the hepatic flexure. It is highly variable both in length (approximately 50 cm long on average) and the extent to which it hangs down anterior to the small bowel between websites of attachment at the right (hepatic) and left (splenic) colic flexures. The splenic flexure lies at a higher level than the hepatic flexure, typically abutting the spleen under the left decrease ribs. The disposition of the transverse colon and extra posteriorly sited flexures ends in the anterior taenia of the ascending (and descending) colon lying inferiorly (see above). Accessory appendicu lar arteries are common; two or extra arteries may supply the appendix. Right colic artery the right colic artery is relatively small and variable in its anatomy (Batra et al 2013). It passes to the proper, throughout the proper psoas main and quadratus lumborum, crossing the best gonadal vessels and ureter, simply posterior to the peritoneal floor of the right infracolic compartment. Near the left aspect of the ascending colon, it divides right into a descending department, which runs down to anastomose with the superior branch of the ileocolic artery, and an ascending branch, which passes up throughout the decrease pole of the best kidney to the hepatic flexure, the place it anastomoses with a department of the center colic artery. It runs steeply downwards, posterior to the splenic vein and body of the pancreas, with the superior mesenteric vein on its proper, and directly anterior to the left renal vein, the uncinate strategy of the pancreas and the third a half of the duode num. It then enters the root of the mesentery of the small intestine and passes obliquely downwards and to the proper, giving off a number of branches to the massive gut. Middle colic artery the center colic artery arises from the best side of the superior mesenteric artery, either separately or in frequent with the best colic artery, simply inferior to the neck of the pancreas, and passes anteriorly and superiorly within the transverse mesocolon, simply to the right of the midline. The left department supplies the terminal part of the midgut and anastomoses with a department of the left colic artery close to the splenic flexure. The marginal artery thus shaped lies a quantity of centime tres from the mesenteric edge of the transverse colon. Sometimes, the center colic artery divides into three or more branches throughout the Ileocolic artery the ileocolic artery arises from the superior mesenteric artery close to the basis of the mesentery of the small intestine, descending inside the mesentery to the best in the path of the caecum, and crossing anterior to the right ureter, gonadal vessels and psoas main. It usually divides into superior and inferior branches, the superior department operating up along the left facet of the ascending colon to anastomose with the right colic artery (or right branch of the middle colic artery) (Veeresh et al 2012). The ileocolic artery offers the most important arterial provide to the caecum; traction on the caecum within the direction of the anterior superior iliac spine will cause the artery to tent up the mesentery, permitting easy identification of the vessel. Here, it gives off a recurrent department, which anastomoses at the base of the appendix with a branch of the posterior caecal artery. The appendicular artery approaches the tip of the organ, at first near to , after which within the edge of, the mesoappendix. The terminal part of the artery lies on the wall of the appendix and may become thrombosed in appen dicitis, leading to distal gangrene or necrosis. In addition, an adjunct middle colic artery is sometimes found arising from the superior mesenteric artery proximal to the origin of the actual center colic artery (Turmezei and Cockburn 2009). Hilum of spleen Tail of pancreas Left renal vein Veins All the branches of the superior mesenteric artery are accompanied by correspondingly named veins. These tributaries drain into the superior mesenteric vein, which ascends to the right of the artery, crossing the third part of the duodenum and uncinate strategy of the pancreas. Behind the neck of the pancreas, on the level of the transpyloric plane (the lower border of the physique of the first lumbar vertebra), it joins the splenic vein to form the portal vein, which ascends behind the first a half of the duodenum to attain the liver. Several tributaries draining into a number of middle colic veins are extremely variable in extent and position. The middle colic veins drain either into the supe rior mesenteric vein, simply earlier than its junction with the splenic vein, or immediately into the hepatic portal vein. The appendicular vein often joins the caecal vein to turn into the ileocolic vein; infection from the appen dix can therefore be carried on to the liver by way of the portal vein. Its position with respect to the spleen is variable: it often lies inferomedial to the decrease pole, forming the colic impression, however it might lie anterior to the splenic hilum, or even a little above. The splenic flexure is often attached to the splenic capsule by a peritoneal ligament and inadvertent downward traction on the flexure during surgery could tear the splenic capsule. The phrenicocolic ligament attaches the flexure to the diaphragm under the inferior pole of the spleen at concerning the level of the tenth rib. The splenic flexure usually adopts a really acute angle such that the tip of the trans verse colon overlaps the start of the descending colon; there could the descending colon is 25�30 cm long and descends from the splenic flexure in the left hypochondrium to the level of the iliac crest, where it curves medially anterior to iliacus to become the sigmoid colon.

Plaquenil 400mg mastercard
Key: 1, 1 subscapularis; 2, triceps brachii (medial head); 3, coracobrachialis; 4, pronator teres (humeral head); 5, widespread flexor origin; 6, supraspinatus; 7, 2 pectoralis main; 8, latissimus dorsi; 9, teres major; 10, deltoid; 11, brachialis; 12, brachioradialis; 13, extensor carpi radialis longus; 14, common extensor origin. Key: 1, infraspinatus; 2, teres minor; three, triceps brachii (lateral head); four, deltoid; 5, brachialis; 6, 3 triceps brachii (medial head); 7, anconeus. Key: 1, head; 2, anatomical neck; three, surgical neck; 4, larger tubercle; 5, 5 lesser tubercle; 6, intertubercular sulcus; 7, shaft. Key: 1, larger tubercle; 2, surgical neck; 3, shaft; 4, radial groove; 5, head; 6 6, anatomical neck. The distal end is customized to the forearm bones on the elbow joint and carries the medial and lateral epicondyles with the articular surfaces for the radius and ulna between them. The shaft of the human (and primate) humerus is comparatively medially rotated with respect to the humeral head, in contrast with quadripedal ancestors; this offers the characteristically higher range of exterior rota tion on the glenohumeral joint than that obtaining in different species. This is mirrored within the spiroidal architecture of the adult humeral medullary cavity, the arrangement and relationship of the posterior compartment of brachial muscle tissue and the radial nerve, and the disposition to long spiroidal fractures caused by exterior twisting forces. With the arm by the facet within the anatomical position, and with the medial and lateral epicondyles in the identical (frontal) airplane. It is necessary to keep in mind this place of the bone when movements of the arm and forearm are thought-about; movements are recorded relative to the trunk (starting within the anatomical position) or relative to the scapula, and you will need to define which method is in use. It accommodates the lengthy tendon of biceps, its synovial sheath, and an ascending department from the anterior circumflex humeral artery. The rough lateral lip of the groove is marked by the bilaminar tendon of pectoralis major, and its medial lip by the tendon and muscular insertion of teres main. The floor of the groove supplies attachment for a frequent upward extension of the tendon of pectoralis major, and for the tendon of latissimus dorsi extra caudally (Dancker 2013). It could be readily palpated laterally and medially, however the muscular tissues of the anterior and posterior compartments obscure the bone to palpation anteriorly and posteriorly. It has three surfaces and three borders, which are only distinct in the path of the elbow joint. Surfaces Proximal finish the proximal finish of the humerus consists of the top, anatomical neck, and the larger and lesser tubercles. The proximal end of the humerus makes up the upper fifth of the length of the bone. A slight roughness indicates the line of capsular attachment of the shoulder joint, apart from on the intertubercular sulcus, where the lengthy tendon of biceps brachii emerges. Medially, the capsular attachment diverges from the anatomical neck and descends 1 cm or extra on to the shaft. Lesser tubercle the lesser tubercle is anterior to and just distal to the anatomical neck. It is palpable via the thickness of deltoid about three cm below the anterior edge of the acromion. The lateral fringe of the lesser tubercle is sharp and types the medial border of the intertubercular sulcus. The transverse ligament of the shoulder (transverse humeral ligament) is connected to the higher aspect of the lateral margin of the tubercle. Greater tubercle 806 the larger tubercle is essentially the most lateral a half of the proximal finish of the humerus and tasks beyond the lateral border of the acromion. The projecting lateral floor of the tubercle presents quite a few vascular foraminae and is roofed by deltoid, producing the traditional rounded contour of the shoulder. A part of the subacromial bursa might cover the the posterior surface, between the medial and lateral borders, is broad, flat and convex distally. The medial head of triceps is attached to the posterior surface over an elongated triangular area, the apex of which is positioned on the medial a half of the bone above the extent of the lower limit of insertion of teres main. The space widens beneath and covers the entire floor virtually down to the lower finish of the bone. The lateral head of triceps is connected to a ridge, sometimes tough, that descends obliquely and laterally above the attachment for the medial head. Above triceps, the axillary nerve and the posterior circumflex humeral vessels wind around the bone on the deep surface of deltoid.
Real Experiences: Customer Reviews on Plaquenil
Ateras, 56 years: A pouch or recess of synovium extends superficial to the free fringe of the pulley fibres so that the free edge varieties a lip protruding into the synovial area. The thoracic splanchnic nerves are subject to appreciable particular person variation in their origin and distribution (Loukas et al 2010).
Rune, 34 years: The lateral or acromial finish of the bone is flattened and articulates with the medial facet of the acromion, whereas the medial or sternal end is enlarged and articulates with the clavicular notch of the manubrium sterni and first costal automotive tilage. Other muscles in the face, jaws, neck and limbs may be concerned, and in severe circumstances, the ventilatory muscular tissues are compromised.
Navaras, 50 years: It acts alone in slow, unopposed supination, and together with biceps brachii in quick or forceful supination. However, if the inhaled particles are abrasive or chemically energetic, they may elude macrophage elimination and damage the respiratory floor, producing fibrosis and a concomitant reduction within the respiratory space.
8 of 10 - Review by D. Trompok
Votes: 152 votes
Total customer reviews: 152
References
- Fenske J, Schwenk T. Obsessive compulsive disorder: diagnosis and management. Am Fam Physician 2009;80(3):239-45.
- Naylor B. Medical, hospital groups oppose GOP health care plan. https://www.npr.org/2017/03/09/519450642/medical-hospital-groups-oppose-gop-health-care-plan. Published March 9, 2017.
- Enerback L, Fall M, Aldenborg F: Histamine and mucosal mast cells in interstitial cystitis, J Neuroimmunol 27:113n116, 1989.
- Lee H, Ryan RT, Teichman JM, et al: Stone retropulsion during holmium:YAG lithotripsy, J Urol 169:881-885, 2003.
- Ea HK, Monceau V, Camors E, et al. Annexin 5 overexpression increased articular chondrocyte apoptosis induced by basic calcium phosphate crystals. Ann Rheum Dis 2008; 67:1617-25.
- Wilhelm M, Kunzmann V, Eckstein S, et al. Gammadelta T cells for immune therapy of patients with lymphoid malignancies. Blood. 2003;102(1):200-206.
- Biederer J, Charalambous N, Paulsen F, et al. Treatment of acute pulmonary embolism: local effects of three hydrodynamic thrombectomy devices in an ex vivo porcine model. J Endovasc Ther. 2006;13:549-560.
- MERCURY Study Group. Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ 2006; 333(7572):779.