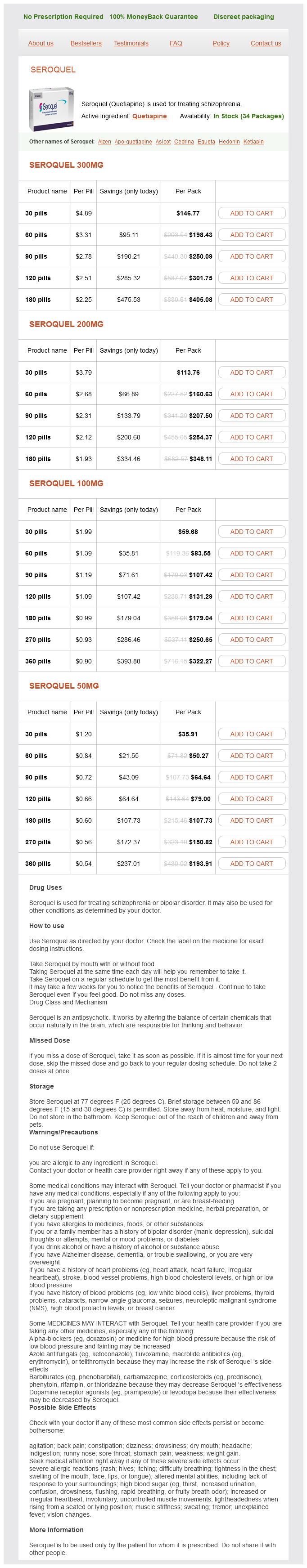
Seroquel dosages: 300 mg, 200 mg, 100 mg, 50 mg
Seroquel packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Buy 50 mg seroquel with visa
Thumb metacarpophalangeal capsulodesis: an adjunct process to basal joint arthroplasty for collapse deformity of the first ray. Metacarpophalangeal and proximal interphalangeal joint accidents of the hand, together with the thumb. Treatment of volar instability of the metacarpophalangeal joint of the thumb by volar capsulodesis. These disruptions are regularly the outcomes of an athletic harm, a fall, or a motorized vehicle accident. The articulating floor of the base of the proximal phalanx is a shallow concavity that gives relatively little intrinsic stability. They fan out from their proximal origins to distal insertions on the lateral and volar side of the base of proximal phalanx. The accessory collateral ligaments act as supplementary helps originating from the palmar side of the metacarpal neck fossa and inserting into the volar plate and the sesamoid on respective sides of the joint. Less severe avulsions might lead to outstanding osteophytes on the dorsoradial aspect of the metacarpal neck, suggesting the prior damage. The stress take a look at could additionally be aided by live fluoroscopy and using a neighborhood anesthetic block. The outcomes of the stress take a look at are primarily based on angular instability of the joint and the quality of the "end point. The dorsoradial facet of the metacarpal head may be outstanding as a result of soft tissue swelling. The slender adductor aponeurosis is interposed between the avulsed ligament�bone and the location of attachment. Images of the contralateral thumb are used for comparability and should reveal subtle joint subluxation. Additionally, a displaced avulsion fracture involving a important portion of the articular floor ought to be lowered and stabilized operatively. An avulsion fracture of the proximal phalanx could be successfully managed by arthroscopic strategies. A regional anesthetic combined with gentle intravenous sedation is usually enough for the procedures detailed beneath. Arthritis Diffuse gentle tissue injury involving a previously asymptomatic however arthritic joint may end up in persistent pain. Preoperative radiograph exhibiting an avulsion fracture on the ulnar collateral ligament insertion website. Postoperative radiograph exhibiting fixation of the fragment and attachment of the ligament using a Kirschner wire and a bone anchor. Palpate the joint after which inject 1 to 2 mL of lidocaine utilizing an 18-gauge needle. Insert a 2-mm full-radius shaver in the ulnar portal and evacuate the hematoma and any minute bone fragments that will forestall visualization. Insert a small probe via the ulnar portal and hook the fragment on its radial facet, inside the fracture site. Preoperative radiographs assist to plan the precise maneuver essential for fracture reduction, but the arthroscopic image will finally determine the course of fragment derotation required to obtain anatomic discount of the joint. Reintroduce the shaver as needed for d�bridement and to help fracture reduction. With the arthroscope in the dorsoradial portal and the shaver in the dorsoulnar portal, arthroscopic d�bridement is carried out earlier than discount of the fragment. Arthroscopic view displaying the Kirschner wire and the fracture fragment before reduction. Inspect the joint, and perform a limited d�bridement and synovectomy as indicated. Less common intrasubstance tears are repaired primarily with 3-0 or 4-0 everlasting suture in a mattress or determine of 8 configuration. Isolate the anatomic insertion site for the right collateral ligament on the volar ulnar base of the proximal phalanx and put together the positioning for ligament attachment by d�briding the remaining delicate tissue all the method down to bleeding bone. Insert a 2-mm or smaller suture anchor into the ready bony website and verify its place with fluoroscopy.
Syndromes
- Fever
- Heavy lifting
- Prolapse of the bladder
- Low blood pressure
- Thyroid level
- Shock
- Cartilage surgery to knee

Order 200 mg seroquel with mastercard
On the other hand, venography of the axillary veins is a simple and accurate method of determining brachial plexus involvement. Large bone tumor (primary bone sarcoma or metastatic lesion) of the proximal humerus and scapula with and intensive gentle tissue part and invasion into the shoulder joint and surrounding muscular tissues. An axillary roll is positioned beneath the axilla to allow full tour of the chest, and a sponge-rubber pad is placed underneath the hip to prevent ischemic harm to the pores and skin in this space. Forequarter amputation entails en bloc removing of the higher extremity together with the scapula and the lateral side of the clavicle. The commonest indications include massive sarcomas or carcinomas of the axillary space with involvement of the bony shoulder girdle or tumor fungation via the axilla. Lymphoma of the shoulder girdle and brachial plexus with a non-union pathological fracture and no response to radiation therapy. Plain radiograph displaying destruction of the proximal humerus and the shoulder joint, in addition to a non-union fracture. Plain radiograph demonstrating very giant delicate tissue mass in the axillary area brought on by extraosseous progress of a Ewing sarcoma. The neurovascular bundle was encased and compressed by the tumor, and the affected person had overt edema of the upper extremity and compromised radial and median nerve capabilities. Axillary venography displaying that the axillary vein is type of completely thrombosed from compression by surrounding tumor. This look has confirmed to be a particularly reliable prognostic discovering of brachial plexus involvement. If axillary venography exhibits axillary vein obstruction, a forequarter amputation almost is at all times required at the time of exploratory surgery. The patient is positioned in a full lateral position and is secured to the operating desk at the hips with tape. An axillary roll is positioned beneath the axilla to enable full excursion of the chest, and a spongerubber pad is placed underneath the hip to forestall ischemic harm to the pores and skin in this area. Intraoperative images exhibiting a domestically recurrent osteosarcoma on the proximal arm and axilla in a 34-year-old affected person E. A 59-year-old woman with a regionally recurrent malignant melanoma extensively involving the arm, axilla, and shoulder that grew quickly despite chemotherapy, immunotherapy, and radiation. The incision begins proximal over the shoulder and extends distally along the axillary border of the scapula and curves towards the midline. The pectoralis main muscle has been transected; this photograph demonstrates the pectoralis minor over the tumor. A giant posterior fasciocutaneous flap following a forequarter amputation for a large fungating tumor of the anterior axillary area. Therefore, a large posterior fasciocutaneous flap has been raised utilizing a element of skin from the posterior two-thirds of the arm. This prolonged posterior fasciocutaneous flap is extremely reliable and could be rotated to shut massive chest wall and anterior defects as properly as the posterior triangle of the neck. Note the flap has lined the large space extending to the midline anterior, to the bottom of the neck, and the adjacent chest wall. Caudally, the incision line is in or near the deltopectoral groove; superiorly, it crosses the tip of the acromion. The last form of the flaps and position of the traces of incision will range according to the individual tumor extent. Caudally, the incision line is in or near the deltopectoral groove; superiorly, the incision line crosses the tip of the acromion. Intraoperative pictures displaying the anterior (B) and posterior (C) arms of the incision. The anterior flap is elevated, exposing the clavicle, acromion, and the overlying origin of the pectoralis main muscle. The origin of the muscle is detached from the clavicle, and an osteotomy is carried out. Occasionally, massive tumors extend to the overlying pores and skin and require en bloc resection with a considerable area of pores and skin.
Seroquel 100 mg order mastercard
Comminution of the metaphyseal cavity or dorsal wall usually suggests a dorsally unstable fracture sample. Fractures with important volar displacement are almost all the time unstable and require some sort of intervention to acquire and maintain a discount till union. Often, this pattern is comminuted and highly unstable and not suited to closed methods of treatment. This sample is characterized by the presence of an ulnar nook fragment that involves the dorsal portion of the sigmoid notch, a major articular fragment, and a proximal shaft fragment. Unstable fractures with advanced involvement of the articular floor to simplify complex articular fractures. However, if the articular surface is in dorsal tilt, the x-ray beam is parallel to the subchondral bone of the dorsal half of the lunate facet and the carpal aspect horizon identifies the dorsal rim (not shown). Depression of the teardrop angle to a value less than forty five degrees indicates that the volar rim of the lunate aspect has rotated dorsally and impacted into the metaphyseal cavity (axial instability sample of the volar rim). The subchondral outline of the articular floor of the distal radius is generally congruent and concentric with the subchondral define of the bottom of the lunate; a uniform joint interval must be current between the radius and lunate alongside the whole articular floor. Note the improved visualization of the articular surface of the bottom of the scaphoid side and the entire lunate facet. Abnormal articular concentricity, indicating disruption across the volar and dorsal surfaces of the lunate facet. Dorsal rotation of the volar rim leads to dorsal subluxation of the carpus from this normal position, inserting the flexor tendons at a mechanical disadvantage, which may have an result on grip strength. In addition to the harm movies, it may be very important reassess postreduction views to decide the character and particular elements of the fracture. Clinical and radiographic evaluations of the carpus, interosseous membrane, and elbow are used to establish the presence of different related accidents that may affect the choice for a particular remedy. Preoperative Planning Extra-articular fractures: a number of options: Volar plating through a volar strategy Dorsal plating via a dorsal method Fragment-specific fixation Radial pin plate (TriMed, Inc. Fixation of dorsal, ulnar nook, and free intra-articular fragments can be carried out by way of a dorsal strategy. Operative Sequence Radial column size is restored first with traction; a transstyloid pin is inserted to maintain the discount if needed. Free intra-articular fragments and the dorsal wall if needed are lowered and stabilized. C-arm If the armboard is radiolucent, the C-arm may be brought in from the end of the armboard and images taken immediately with the wrist on the armboard. Leaving the distal 1 cm of sheath intact, open the first dorsal compartment proximally and mobilize the tendons. If needed, the dissection may be continued by way of the floor of the incision to expose the volar floor. Alternatively, create an ulnar pores and skin flap superficial to the artery and proceed the exposure via a regular volar approach. Sweeping tenotomy scissors to elevate radial pores and skin flap off first dorsal compartment. Develop the interval between the third and fourth compartment tendons for access to dorsal wall and free, impacted articular fragments. Develop the interval between the fourth and fifth extensor compartments to acquire access to the ulnar nook fragment. To acquire entry to the radial column through a dorsal publicity, lengthen the incision as wanted and elevate a radial subcutaneous flap and supinate the wrist. To gain access to the distal ulna, prolong the incision as needed and elevate an ulnar subcutaneous flap. If entry to the radial column is required, elevate a radial subcutaneous flap superficial to the radial artery and first dorsal compartment tendon sheath. With blunt finger or sponge dissection, develop the plane on the superficial floor of the pronator quadratus. Do not dissect more than 1 to 2 mm beyond the distal radial ridge to keep away from detaching the volar wrist capsule. Release the tendon sheath of the primary dorsal compartment proximally, leaving the last 1 cm of tendon sheath intact. Retract the tendons of the first dorsal compartment dorsally or volarly as wanted. If needed, structural bone graft could be inserted via the radial fracture defect.

100 mg seroquel with amex
Distal femoral osteogenic sarcoma: rules of softtissue resection and reconstruction at the side of prosthetic alternative (adjuvant surgical procedures). Function after elimination of varied hip and thigh muscular tissues for extirpation of tumors. Functional reconstruction of the extensor mechanism following huge tumor resections from the anterior compartment of the thigh. Chapter 31 Adductor Muscle Group (Medial Thigh) Resection Jacob Bickels, Martin M. Tumors arising throughout the adductor compartment are often extraordinarily massive at presentation. As they enlarge they typically displace the superficial femoral and profundus vessels, and they may contain the extrapelvic flooring musculature (obturator fascia) and bone (superior and inferior pubic rami and ischium) and even extend extracompartmentally to the medial hamstrings or the psoas muscle and the adjoining hip joint. Such large tumors had been historically handled with amputation (ie, hemipelvectomy). However, effective chemotherapy and radiotherapy regimens have allowed limb-sparing resections to be performed at that site with low charges of local tumor recurrence. Lipomas and low-grade liposarcomas, that are the most typical tumor type at that website, are normally removed simply with their enveloping capsule with out having to manipulate the vascular bundle. High-grade soft-tissue sarcomas, nonetheless, might grossly adhere to and surround the vascular bundle and require partial or complete resection of the concerned bundle section. Therefore, a limb-sparing tumor resection at that website begins with dissection and preservation of the superficial femoral vessels. Large high-grade sarcomas normally necessitate ligation of the profundus femoris artery. The surrounding adductors are then detached from their origin along the inferior and superior pubic rami and ischium and removed en bloc with the tumor. The gentle tissue defect remaining after tumor resection is usually reconstructed by transferring the sartorius muscle and the remaining medial hamstrings. The bony constructions of the pelvic floor are the closest margins for big sarcomas that arise within this muscle group. Rarely, proximal adductor tumors might lengthen as a dumbbell across the ischium into the ischiorectal fossa. In these instances, we advocate induction chemotherapy or isolated limb perfusion and repeated staging research earlier than a definitive determination is made regarding amputation. The profundus femoris artery, then again, is often involved and have to be ligated because it passes by way of the adductor brevis. The obturator artery and nerve, which pass via the obturator fascia, are routinely ligated. In gentle of the above, preoperative vascular analysis of the patient ought to embrace direct questioning about intermittent claudication, limb swelling, and deep vein thrombosis. Compartmental muscular tissues come up from the pelvic flooring and the medial facet of the ipsilateral pelvic ring (symphysis pubis, inferior pubic ramus, ischium, and obturator fascia) and attach distally to the linea aspera and the medial facet of the distal femur. The superficial femoral artery passes along the anterior and lateral margins of the whole compartment and varieties the lateral border. Coronal part exhibiting a dumbbell-shaped extension across the ischium into the pelvic cavity. Although the vessels are considerably displaced, a plane of dissection is clear between them and the tumoral mass. Biplanar angiography, especially in sufferers older than forty, ought to be accomplished to evaluate the patency of the superficial femoral artery: ligation of the profundus artery without a patent superficial femoral artery will lead to a nonviable extremity. In the previous, angiography was additionally used preoperatively to outline the course of the vascular bundle within the affected thigh and to assess the likelihood of vascular reconstruction. This incision permits giant anterior and posterior flaps to be developed to visualize the vastus medialis, the sartorial canal, and the complete adductor compartment. The sartorial canal is opened proximally to establish the frequent femoral artery before ligating the profundus vessels. The muscle tissue are detached from their origin (superior and inferior pubic rami) and alongside the obturator foramen. The incision extends from the proximal border of the inguinal area simply inferior to the sartorius muscle and parallels the muscle to the posteromedial facet of the knee, to embrace the earlier biopsy site. Large anterior and posterior fasciocutaneous flaps are elevated and retracted anteriorly to expose the vastus medialis and the sartorial canal and posteriorly to the lower fringe of the adductor muscle group. The adductor magnus and longus are detached from their insertions on the femur all through its length to the adductor hiatus.

Discount seroquel online visa
If the tumor approaches the vessels, then the sheath is eliminated and despatched for a frozen section examination. Resection of the adjacent vascular sheath is routinely performed, similar to kind 1 tumors. The initial approach is just like that for types 1 and a couple of but in addition involves resection of the superficial femoral artery and vein. The artery must be reconstructed, either with a Gore-Tex graft or the ipsilateral saphenous vein. The sartorius is resected with the tumor if essential from an oncologic point of view. Soft tissue reconstruction with a gracilis muscle transfer affords good delicate tissue coverage of the vessels of the sartorial canal and is taken into account crucial. The lateral arm of the incision is made alongside the decrease border of the biceps femoris muscle because the peroneal nerve is initially picked up just below the deep fascia as a satellite tv for pc of the biceps muscle. The tumor is in shut proximity to the sciatic nerve above it and the popliteal artery and vein just below it (vessel loops). Care must be taken to not open the popliteal fascia whereas developing the flaps to cut back the danger of neurovascular injury. Release of the gastrocnemius heads, which are then reflected distally for maximal exposure. Tenodesis of the heads of the gastrocnemius and the hamstring muscular tissues, forming a muscular coverage over the popliteal vessels and nerves. The peroneal nerve is first identified simply medial to the biceps muscle, just under the deep fascia. The deep fascia is then opened longitudinally and the sciatic nerve is identified between the medial and lateral hamstrings. The four muscular tissues that make up the "diamond" of the popliteal house at the moment are identified: the medial and lateral hamstrings proximally and the medial and lateral gastrocnemius muscles distally. The popliteal vessels and the tibial nerve are mobilized and a vessel loop is positioned round them for distal control. The sciatic nerve is then mobilized, each the peroneal and the tibial nerve parts. The popliteal artery and vein are identified proximally close to the medial hamstrings deep in the fossa as they enter from the adductor foramen. Careful dissection and mobilization of the vascular and nerve buildings are then performed. The medial or lateral head, or both, of the gastrocnemius muscular tissues may be released from their origins on their respective femoral condyles to help in the exposure. Similarly, the semimembranosus or biceps femoris muscle could additionally be released for better publicity. If the tumor extends proximally (between the hamstrings or distally between the gastrocnemius muscles), then the corresponding muscle have to be released to acquire a wide excision. The popliteal vessels are usually displaced and never involved by tumor, except a leiomyosarcoma is arising from them. The tumor is resected solely after all the above constructions are identified and mobilized. Sheaths of the adjacent nerves or vessels are removed and sent for frozen part examination to determine whether additional resection is required. Soft tissue closure is necessary to cowl and fill the popliteal house to forestall wound problems. The medial and lateral gastrocnemius heads are tenodesed to one another, masking the distal portion of the popliteal space and the neurovascular buildings. Similarly, the medial hamstrings are tenodesed to the biceps femoris muscle to close over the proximal popliteal area. Both the gastrocnemius and the hamstrings are then sutured collectively to make a nice muscle closure of the entire popliteal area. Angiography Type three resections Vascular control Neurologic examination of femoral and sciatic nerve perform Tumors are categorized as sorts 1, 2, or 3 (discussed earlier).
Cassia Cinnamon. Seroquel.
- Are there safety concerns?
- Loss of appetite, muscle and stomach spasms, bloating, intestinal gas, vomiting, diarrhea, common cold, impotence, bed wetting, menstrual complaints, chest pain, high blood pressure, kidney problems, cancer, and other conditions.
- What is Cassia Cinnamon?
- How does Cassia Cinnamon work?
- Are there any interactions with medications?
- Dosing considerations for Cassia Cinnamon.
- Diabetes.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96963

Discount 300 mg seroquel with amex
A hook probe could be inserted dorsally in the midcarpal radial portal for palpation. The tendons are retracted to the radial side and the radiocarpal joint space is identified with a 22-gauge needle. Care is taken to situate the portal beneath the ulnar edge of the flexor tendons and to apply retraction in a radial path alone to avoid injury to the ulnar nerve and artery. Direct visualization of the foveal attachment prevents accidental injury to this construction. In ideal instances, the conjoined tendon of the dorsal radioulnar ligament, ulnar collateral ligament, and palmar radioulnar ligament could be visualized. This portal is less complicated to penetrate and ought to be used initially to forestall chondral harm from insertion of the trocar. The forearm is held in supination to relax the dorsal capsule, to move the ulnar head volarly, and to lift the central disc distally from the pinnacle of the ulna. Reducing the traction to 1 to 2 pounds permits better views between the ulna and the sigmoid notch by decreasing the compressive pressure caused by axial traction. The joint house is entered by inserting a 22gauge needle horizontally on the neck of the distal ulna. Entry into this portal provides views of the proximal sigmoid notch cartilage and the articular floor of the neck of the ulna. Wrist traction often diminishes through the process and ought to be readjusted as needed to avoid scraping the articular floor. Use of a standard methodologic strategy ensures a complete and thorough examination. After diagnostic arthroscopy, with or with out d�bridement, the patient is splinted for comfort for a short period of four to 7 days. Active wrist motion is inspired after this era and sufferers are allowed actions of day by day residing, adopted by gradual strengthening. The palmar cutaneous department of the ulnar nerve is at risk with the volar radial portal, although the interposed flexor carpi radialis tendon mitigates this risk. Venous bleeding, loss of wrist motion (especially forearm supination), issues related to fluid extravasation, and infection are general dangers attendant to any arthroscopic process. These could be minimized by fastidious surgical method, aggressive rehabilitation as essential, and diligent followup within the early postoperative interval. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal finish of the radius. Chapter 4 Open Reduction and Internal Fixation of Diaphyseal Forearm Fractures Michael R. Surgical reconstruction of diaphyseal forearm fractures requires precise realignment of each radius and ulna to minimize problems and maximize operate. Ingenious surgical approaches have been described that enable the surgeon to follow outlined internervous planes to the bones for inside fixation. The design of the forearm permits close to 180-degree rotation combining with considerable elbow flexion�extension and wrist circumduction. To obtain this, the ulna is enlarged proximally, making it a principal bone of the elbow, and is smaller distally, whereas the reverse is true for the radius, with the enlarged radius being the primary articulation with the carpus. The result for the diaphysis of every bone is that the proximal ulna is metaphyseal for about 25% to 30% of its length however distally less than 10%, with the reverse holding true for the radius. Implant design has taken these variations under consideration, with many whole techniques obtainable for metaphyseal distal radius and proximal ulna fractures. The importance of maintaining the radial and ulnar heads has only lately been understood. This allows the ulnar head to move out of the finest way of the rotating radius distally. Schemitsch and Richards22 quantified the importance of the distal of the 2 bows within the radius. Restoration of this bow is the only most important step in reconstruction of the forearm after diaphyseal fracture. To determine whether or not the bow has been restored after osteosynthesis, draw a line from the biceps tuberosity to the sigmoid notch.
100 mg seroquel order with mastercard
Radiograph of the resected specimen showing complete involvement of the hemipelvis. A giant tumor mass is seen arising from the obturator internus muscle (solid arrows). The procedure is begun with dissection of the exterior rotators and osteotomy of the femoral neck, per total hip process. Incise the hip capsule peripherally with dissection of the sciatic nerve proximally to the sciatic notch. The anterior and posterior columns are exposed to permit osteotomy of the acetabulum. Posterior column osteomy requires cautious exposure and retraction of the sciatic nerve and gluteal vessels. Once the cement (polymethylmethacrylate) is prepared, the gauze is eliminated, and the femoral prosthesis is cemented inside the proximal femur. Composite Allograft Acetabular Reconstruction Femoral element: ream and place the uncemented femoral part by way of the posterior lateral approach earlier than proceeding with iliac osteotomy resection. Acetabulum: ream the allograft for the acetabular part and place the acetabular part (cement and screws) into the allograft to confirm graft and acetabular orientation in situ with radiography before screw or cement fixation. Check acetabulum positioning with radiographs earlier than and after fixation or cementation. Orient the iliac graft earlier than confirming the acetabular orientation, and repair the graft with a reconstruction plate and screws. Use an extended polyethylene acetabular rim and think about a big femoral head (32�36 mm) to improve postoperative stability. Using the inguinal ligaments, reconstruct the abductors, particularly if a trochanteric osteotomy was done. Perform pelvic closure at the iliac crest and inguinal canal with wound drainage catheters. The base part length ought to be determined by the space between the ilium and femoral neck cuts, as a end result of the length indicated on the base part is the total length from the notch of the saddle to the femoral collar. The surgeon should be succesful of reattach the abductor mechanism to its anatomic position on the osteotomized higher trochanter. A trial reduction can also determine areas where the saddle component might impinge on the prevailing notch throughout intraoperative vary of motion. These areas can be additional contoured with a high-speed burr to prevent impingement, which may result in restricted motion or dislocation. Hip movement (flexion to no much less than 90 degrees, extension to 30 levels, abduction to forty five levels, adduction to neutral, and rotation) should be possible with out proof of impingement or dislocation. The notch ought to be placed within the thickest area of the remaining bone (usually medial). Preparation of the Proximal Femur the proximal femur is prepared as for a standard femoral component. The intramedullary canal of the proximal femur is reamed to accept the largest-diameter stem and allow for a 2-mm circumferential cement mantle. Once reaming is completed, and the appropriate-sized stem (diameter and length) is chosen, a distal femoral cement the osteotomized greater trochanter and abductors are reattached to their authentic location using cables. If the higher trochanter was included within the resected specimen, the abductor mechanism is reattached to the prosthesis utilizing 3-mm Dacron tapes or a cable system. Soft tissue tension and prosthetic stability are again tested once the abductor mechanism reconstruction is complete. The piriformis and quick external rotator muscles are brought forward and reattached to the proximal femur (or prosthesis). Pelvic closure includes attachment of the inguinal canal and belly wall to the symphysis pubis and lateral iliac crest. Soft tissue pressure and prosthetic stability are tested again once the abductor mechanism reconstruction is complete. The gluteus maximus is then reattached to its insertion using nonabsorbable suture.
Cheap seroquel 100 mg without a prescription
This is the deformity that changed a traditional flexible flatfoot right into a painful flatfoot. The lateral view demonstrates dorsiflexion of the talus, alignment at the talonavicular joint, correction of the talo�first metatarsal angle, and normalization of the calcaneal pitch. A well-padded short-leg non-weight-bearing forged is utilized and bivalved to allow for swelling overnight. The affected person is discharged from the hospital the following day after the bivalved cast is overwrapped with forged material. This may be averted by lengthening the peroneus brevis, releasing the aponeurosis of the abductor digiti minimi, releasing the plantar calcaneal periosteum and lengthy plantar ligament (not the plantar fascia), and pinning the calcaneocuboid joint in a retrograde style earlier than the osteotomy is distracted. This may be averted by performing the procedures listed just above and by releasing the entire dorsal talonavicular joint capsule. Persistent equinus may be averted by lengthening the contracted Achilles tendon or gastrocnemius tendon. Persistent supination deformity of the forefoot on the hindfoot may be prevented by identifying it after the calcaneal lengthening and heel twine lengthening. It has been shown to appropriate all elements of even severe valgus�eversion deformity of the hindfoot, restore perform of the subtalar complex, relieve symptoms, and, at least theoretically, protect the ankle and midtarsal joints from early degenerative arthrosis by avoiding arthrodesis. Implications of subtalar joint anatomic variation in calcaneal lengthening osteotomy. Calcaneal lengthening for valgus deformity of the hindfoot: results in children who had extreme, symptomatic flatfoot and skewfoot. An equinus deformity is either congenital or acquired and could be dynamic or rigid. Achilles or gastrocsoleus contracture usually occurs in combination with other delicate tissue contractures. From here, the Achilles tendon is joined by tendon fibers from the posterior side of the soleus as the tendon programs distally. The tendon is broad proximally and then becomes rounded at the midsection when it undergoes a 90-degree internal rotation earlier than its insertion on the posterosuperior third of the calcaneus. The insertion footprint is delta-shaped, and a small portion of the fibers course distally to meet the origin of the plantar fascia. The proximal portion is provided by branches from inside the gastrocnemius muscle. Instead, the encircling paratenon, comprising loose connective tissue, supplies the relaxation of the blood provide via branches from the posterior tibial artery and, to a lesser diploma, the peroneal artery. One is subcutaneous, positioned between the skin and tendon, and the other is deep, positioned between the tendon and the calcaneus. Acquired equinus deformity secondary to cerebral palsy results from muscle spasticity or imbalance, resulting in subsequent contracture of the Achilles tendon and gastrocsoleus complex. Muscle imbalance and spasticity in spastic diplegic cerebral palsy usually results in equinoplanovalgus deformity. Muscle imbalance and spasticity in spastic hemiplegic cerebral palsy often leads to equinus or equinovarus deformity. Compensatory stability mechanisms to assist preserve ambulation in sufferers with Duchenne muscular dystrophy also might result in equinus deformity. Posttraumatic equinus can be a results of severe burns and posterior scar contracture, postburn positioning, anterior leg muscle loss, or continued tibial development in a inflexible scar. Posterior view of Achilles tendon, demonstrating 90degree rotation of tendon fibers from posterior to medial and anterior to lateral. Despite both conservative and surgical treatments, the deformity can recur as a result of persistent spasticity, muscle imbalance, or limb progress. Equinus deformity leads to abnormal gait due to altered ankle range of motion and decreased ankle plantarflexion moment during terminal stance. It may end up in chronic ache, poorly fitting footwear, callosities on the plantar forefoot, and potential pores and skin ulceration in sufferers with altered sensation.

200 mg seroquel visa
In the presence of scapholunate injury, sharp pain is elicited on the scapholunate area, representing dorsal subluxation of the scaphoid. Scaphoid shift test9: If the scapholunate ligaments are utterly torn, the proximal pole might sublux dorsally out of the radius, inducing ache on the dorsoradial facet of the wrist. This take a look at has low specificity: occult ganglia, hyperlaxity, or radioscaphoid degenerative arthritis may produce comparable signs. Three-ligament tenodesis for the therapy of scapholunate dissociation: Indications and surgical approach. A foreshortened look of the scaphoid with the scaphoid tuberosity projected within the type of a hoop over the distal two thirds of the scaphoid (ring sign) indicates rotatory subluxation of the scaphoid. Lateral radiographic view Increased scapholunate angle in contrast with the contralateral side. For this to be significant, the wrist needs to be in strict neutral alignment and neutral prono-supination. It is also helpful in describing the degree of harm to the interosseous ligaments. Complete disruption of scapholunate ligaments, the dorsal one being nonetheless reparable, with good therapeutic potential. Its contraction generates a dorsally directed vector to the unstable scaphoid that stops its collapse into flexion. Arthroscans (tomograms taken after three-compartment injection of dye) are very helpful to assess cartilage status. Best-quality magnetic resonance imaging could present helpful accent data relating to bone vascularity, synovitis results, and gentle tissue standing. Approach An 8-cm dorsal zigzag, lazy S, or longitudinal incision of the pores and skin and subcutaneous tissue is centered on the tubercle of Lister. The dorsal sensory branches of the radial and ulnar nerves are recognized and protected. The extensor retinaculum is split along the third compartment and the extensor pollicis longus tendon is retracted radially. Indeed, proprioception re-education of this muscle may be helpful in stage 1 scapholunate dissociation. A radially primarily based capsular flap is created by incising the dorsal capsule along the fibers of each the dorsal radiotriquetral ligament and the dorsal intercarpal ligament. Once the capsular flap is retracted radially, the scapholunate injury may be inspected (arrow) and a final therapeutic determination may be made. The dimension of graft harvested is determined by the size of the scaphoid and bone tunnel created. While maintaining the proximal pole of the scaphoid reduced on its fossa, two Kirschner wires are passed throughout the scaphocapitate joint. Later stretch of the tenodesis is likely, by which case the scaphoid will get well its ideal alignment of 45 degrees. The capsular flap is passed underneath the tenodesis and reattached to its origins by absorbable sutures. The extensor pollicis longus is often left superficial to the extensor retinaculum. Note the placement and direction of the bone tunnel as well as the placement of the suture anchor. So as to not injury the medial or lateral articular surfaces of the scaphoid, we recommend using a 2. The dorsal radiotriquetral ligament is used as a pulley to tension the ligament strip. Some sutures are also positioned connecting the capsule and the tendon loop to re-establish the traditional capsular attachment to the dorsum of the scapholunate joint. A trough has been carved onto the dorsal cortex of the lunate and a suture anchor inserted at that location. A slit has been developed along the fibers of the dorsal radiotriquetral ligament. Drill a Kirschner wire from dorsal to palmar and from proximal to distal, aiming on the tuberosity. The bone tunnel dimension, therefore, depends on the tendon graft thickness and likewise on the scale of the scaphoid. A second Kirschner wire enters from the palmar-radial nook of the scaphoid tuberosity, aiming at the lunate.

Seroquel 100 mg order without a prescription
A longitudinal osteotomy that will increase the surface area of the flap can function an onlay graft to augment the therapeutic process for partial cortical defects. Part of the soleus or the flexor hallucis longus muscular tissues can be included with the flap to reconstruct delicate tissue defects and cover exposed bone. The blood provide and drainage of the fibula are associated to the peroneal artery and two peroneal veins, which observe a course parallel to the fibula. The former relies on a nutrient artery that stems 6 to 14 cm from the peroneal bifurcation; the latter relies on multiple periosteal branches alongside the fibular diaphysis. If a protracted segment is required and the osteotomy is close to the lateral malleolus, screw fixation to the tibia is suggested to stop valgus deformity and ankle instability. A pores and skin paddle can be transferred concurrently to facilitate protection of concomitant massive delicate tissue defects and to allow patency of the pedicle anastomosis to be monitored. A proximal fibular graft that includes the proximal fibular epiphysis and is predicated on the anterior tibial vascular pedicle may be used for joint reconstruction and preservation of longitudinal growth in youngsters after intra-articular resection of bone tumors. When the periosteal vessels are transected, the bone survives on its endosteal system. This flap is based on the anterior tibial vascular flap or the descending geniculate artery and is mostly used for reconstructions after resections of the proximal humerus and distal radius. If those research are inconclusive, angiography or magnetic resonance angiography is carried out. The latter is carried out 2 years after tumor resection if there has been no tumor recurrence or lung metastases. The first team, which is responsible for tumor resection (blue team), is positioned along the medial or lateral side of the recipient extremity. If tumor resection is finished from the medial aspect of the extremity, a surgeon could be positioned at that facet. Imaging of the recipient site ought to provide details about the scale of bone (length and diameter) and delicate tissue defects remaining after tumor resection, thus permitting the selection of the suitable sort and size of fibular flap to be used. Imaging of the donor website should include the whole leg and is aimed toward excluding fibular deformity and figuring out maximal flap length. Reconstruction of such defects of the decrease extremity requires graft material of a bigger diameter because of the additional mechanical help wanted. A double-barrel fibular flap can be utilized to reconstruct femoral and tibial defects of as a lot as thirteen cm. Longer defects might require the assist of an allograft, which supplies the initial stability required for bone therapeutic, graft incorporation, and subsequent fibular hypertrophy. Furthermore, in cases of failed vascular anastomosis, the mixed fibular�allograft construct remains to be similar to a number of cortical allogenic struts with a comparatively good likelihood of success, especially if dependable fixation is achieved. The technique of combined reconstruction with an allograft and the vascularized fibula, as described by Capanna and colleagues, provides such stability and is the preferred methodology of reconstruction that we use for long intercalary defects of the decrease extremities. Diaphyseal tumor is resected with wide margins, leaving an extended intercalary bone defect. Plain radiograph of the arm exhibiting considerable bone loss and pathologic fracture associated with acute osteomyelitis of the humeral diaphysis. After tissue sampling and cultures, administration of intravenous antibiotics, and resolution of acute manifestations of infection, the patient underwent resection of the contaminated bone tissue, leaving a protracted intercalary bone defect. A pores and skin graft, usually taken from the thigh of the donor extremity, is used to cowl the pores and skin defect in that leg. The peroneal tendons should be well lined by muscle bulk to enable a protected pores and skin graft take. An intercalary fibular segment, 6 cm longer from the bone defect, is eliminated with its nutrient vessels and its periosteal cuff. If a big skin defect is anticipated on the tumor resection site, the fibular graft is removed with an overlying pores and skin island, which is used to cover that defect and to monitor flap viability. An intramedullary nail can be used if the allograft medullary canal is wide enough to contain each the nail and the fibular graft. Care is taken to stop harm to the nutrient vessels of the fibula by these screws. The fibula can be placed in an intramedullary location, contained in the allograft or parallel to it.
Real Experiences: Customer Reviews on Seroquel
Goran, 63 years: Plate fixation permits for compression throughout the allograft�host junctions, which probably improves therapeutic.
Daryl, 45 years: Fitting for an initial or temporary prosthesis soon after wound therapeutic and swelling decision is most often related to elevated prosthetic use.
Treslott, 25 years: Pelvic metastases are treated both with curettage and reconstruction with cemented hardware or by wide resections.
Knut, 24 years: Malawer; C: Reprinted with permission from Cancer: Principles and Practice of Oncology, fifth ed.
Jorn, 27 years: Positioning the patient is under anesthesia and within the supine position with hips and knees flexed at 30 degrees for low again comfort.
Sanuyem, 33 years: Excision of the coalition is contraindicated if greater than 50% of the joint surface is coalesced or in the presence of subtalar arthritis.
Tippler, 56 years: A notch is made within the supra-acetabular roof or remaining ilium for the saddle prosthesis to sit in.
Gembak, 26 years: Contiguity with a synovium-lined house is uncommon, and, occasionally, lymphatic spread happens.
10 of 10 - Review by X. Pyran
Votes: 50 votes
Total customer reviews: 50
References
- Penna C, Mancardi D, Raimondo S, et al: The paradigm of postconditioning to protect the heart, J Cell Mol Med 12:435, 2008.
- Chen-Scarabelli C, Scarabelli TM: Neurocardiogenic syncope. BMJ 329:336, 2004.
- Neoptolemos JP, Stocken DD, Friess H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med 2004;350(12):1200-1210.
- Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 2014;383(9930):1721-1730.
- Wieling W, Ganzeboom KS, Saul JP. Reflex syncope in children and adolescents. Heart. 2004;90:1094-1100.
- Rao BNS, Anderson RC, Edwards JE: Anatomic variations in tetralogy of Fallot. Am Heart J 1971; 81:361-365.
- Evans R, Mullally DI, Wilson RW. National trends in the morbidity of asthma in the U.S. Chest 1987; 91: Suppl. 6, 65S-74S. 11.